MM Curator summary
The bill that would cover kids who don’t have citizenship documentation was modified to not give politicians running for re-election issues.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
Gov. Phil Murphy announced his intention to expand New Jersey’s Medicaid program to cover the state’s nearly 90,000 uninsured children — including those who are undocumented — as part of his budget address in February. He highlighted his “cover all kids” pledge again in late March at an event in Passaic with U.S. Rep. Bill Pascrell (D-9th) and a half-dozen state legislators and administration staff.
Last Tuesday, Murphy privately signed a revised “cover all kids” bill — which eliminates waiting periods and out-of-pocket costs for most families and provides $20 million to help cover the state’s additional costs — with no statement or fanfare. It was one of eight spending measures that officials said needed his OK before he approved the state’s $46.4 billion spending plan for the 2022 fiscal year, which began Thursday.
While the changes to Medicaid, also known as NJ FamilyCare, will benefit tens of thousands of low-income families, it is not clear how much — or how soon — it will truly help immigrant children. Advocates estimate there are at least 53,000 uninsured kids in New Jersey who qualify for the program economically but are not enrolled, and more than 18,000 of those children are undocumented. Advocates say the number of undocumented children could be much higher because no one is exactly sure how many are living in New Jersey.
No reference to undocumented kids
Unlike previous versions of the bill, the one passed almost unanimously by the Senate and Assembly and signed by Murphy does not mention undocumented or immigrant children. According to several people involved with the process, the language was changed so that lawmakers — who are all up for reelection this year, along with the governor — did not have to be on record voting for a measure that uses public dollars to fund health insurance for undocumented individuals.
Longtime legislative champions of expanding the Medicaid program to include undocumented youngsters said in a statement that the COVID-19 pandemic underscored the importance of insurance coverage and access to proper medical care. They also suggested their work was not done.
“We must keep working towards our goal of providing New Jersey families with quality, affordable health insurance if we want as many residents as possible to receive the care they both need and deserve,” read the statement from Sen. Joe Vitale (D-Middlesex) and Assembly Democrats Yvonne Lopez (Middlesex), Dan Benson (Mercer) and Gordon Johnson (Bergen). “Eliminating wait times and premiums while further promoting this important program will help us achieve this goal.”
Cumbersome process
Some stakeholders said that parents will now be able to enroll children who lack legal residency, but the new process is cumbersome for both the family and state regulators. Under the changes, parents of undocumented children would need to sign them up through a revised FamilyCare Advantage program, in which they are required to pay the full cost of the coverage, and then could apply for a “hardship waiver” to excuse these expenses after they were enrolled.
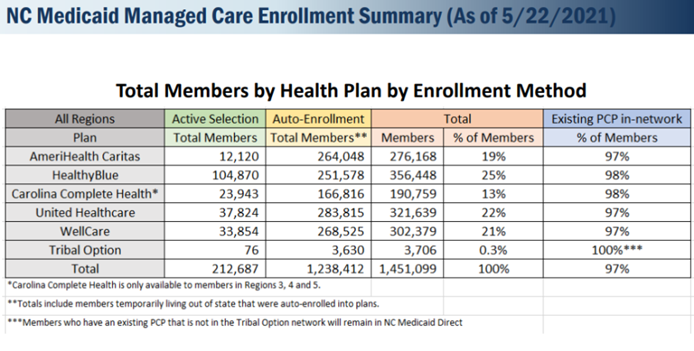
Administration officials said providing health insurance to undocumented children remains a priority for Murphy and noted the plan was proposed in two phases, with the second — focused on immigrant youngsters — still pending. Participation in Medicaid, which now covers nearly 2 million New Jerseyans, grew 17% between March 2020 and March 2021, according to state figures.
The state Department of Human Services (DHS), which oversees Medicaid, did not issue a formal statement on Murphy’s signing of the bill, but acting Commissioner Sarah Adelman added her support on Twitter. Adelman, who previously worked with the New Jersey Association of Health Plans, praised the 15-year effort of sponsors and advocates and noted “We will #CoverAllKids.”
‘This new expansion of NJ FamilyCare puts New Jersey one big step closer to universal coverage for all, starting with our kids.’
In a written response to questions from nonpartisan legislative staff about spending on Medicaid, DHS officials said this spring that state officials will begin planning how to include undocumented children this year, but coverage for these families may not be available until the start of fiscal year 2023 next summer. The department also estimated the cost of this year’s changes could reach nearly $70 million, far more than the $20 million provided in the new budget.
No immediate access?
The DHS timeline squares with the expectations of Maura Collinsgru, the health care policy leader at New Jersey Citizen Action, one of several groups that have long fought to expand Medicaid access, especially for children. A plan unveiled in 2018 by New Jersey Policy Perspective (NJPP), another advocate for expansion, outlined mechanisms similar to those Murphy approved and predicted the changes would cost less than $70 million annually.
“This new expansion of NJ FamilyCare puts New Jersey one big step closer to universal coverage for all, starting with our kids,” something now in place in seven other states, Collinsgru said. “If the pandemic taught us anything, it is having access to health care is essential to our health and economic well-being. By increasing access to coverage, New Jersey can help close the health and wealth gaps that persist in communities of color.”
The new law (S-3798) eliminates a 90-day waiting period for some children to access Medicaid and ends the use of premiums or copays for families who earn less than 350% of the federal poverty level, or less than $6,400 a month for a family of three. It also calls for state officials to enhance and coordinate public outreach around Medicaid and the state’s health insurance exchange, which sells subsidized commercial plans to those who earn too much to qualify for Medicaid but aren’t covered through work.
How it would work
The changes also restart the FamilyCare Advantage program, which allows those who earn more than 350% of the poverty level to purchase this state coverage for their children at cost. This part of Medicaid, which had been unfunded for years, could be used to insure undocumented children, some stakeholders said, but the cost could also be prohibitive for some immigrant families. A “hardship waiver” process was also added to the law, but applying for this option requires additional time and paperwork.
While it does not mention undocumented children in the way previous versions of the legislation did, the law Murphy signed clearly notes: “No child who applies for enrollment in the program who otherwise meets the eligibility criteria for enrollment shall be denied immediate enrollment for any reason.”
That brings hope to many of those who have long advocated to provide undocumented children better insurance options. “All kids in New Jersey deserve access to affordable, high-quality health coverage,” said Brittany Holom-Trundy, an NJPP senior policy analyst. She praised the state for making “an important investment in the state’s future and the long-term health of New Jersey families,” and said she looks forward to working with the administration and health care leaders on “building the best health care system possible for all children in the Garden State.”
Clipped from: https://www.njspotlight.com/2021/07/without-saying-so-nj-expands-medicaid-to-undocumented-children/