MM Curator summary
[MM Curator Summary]: CMS has now provided detailed guidance on how states should deal with eligibility determinations once the PHE is declared over.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
During the COVID-19 Public Health Emergency (PHE), insurers, health technologies, and certain FDA-regulated products were provided various flexibilities in their offering of care. Now the Biden administration is beginning a “return to normal operations” with the release of state guidance that provides up to 12 months to ensure eligibility and renewal reviews of individuals who remained covered under Medicaid during the pandemic. Without appropriate planning, this could result in a disruption of coverage as states begin to verify and renew individuals covered under Medicaid and the Children’s Health Insurance Program (CHIP).
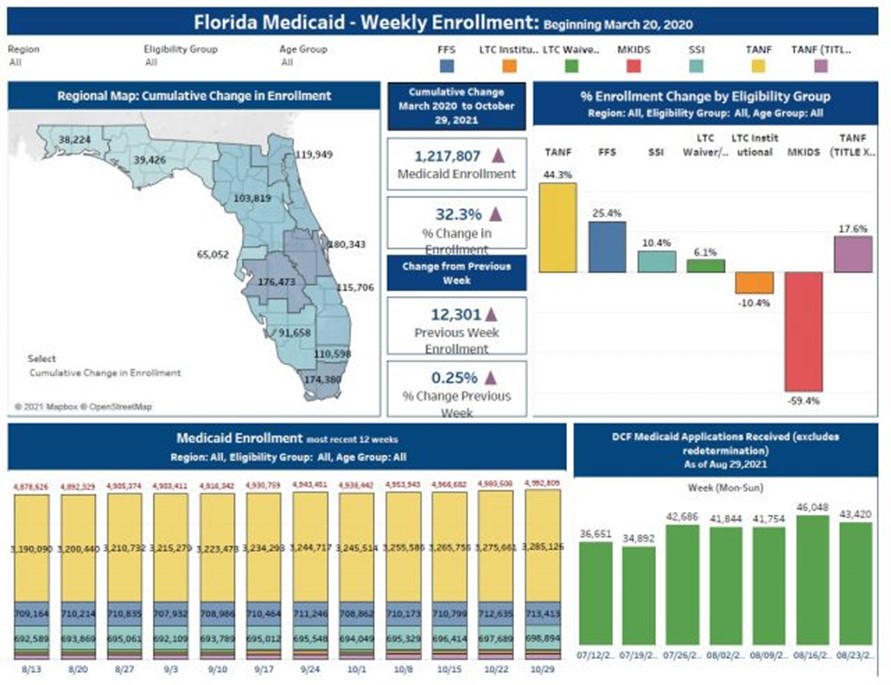
During the pandemic, states were provided incentive payments to maintain continuous enrollment for all individuals enrolled in Medicaid. It is estimated that over 40 million children were enrolled in Medicaid or CHIP during the pandemic. It is also estimated that up to 15 million people, including 6 million children, may be at risk of losing this coverage when eligibility determinations are back in place.
This new guidance sets some specific criteria for states to plan and implement a smooth transition to ensure that individuals enrolled in Medicaid are in fact eligible. The following are key issues established in this guidance for states – that could affect individuals, providers, and plans:
- States have been receiving a temporary 6.2% increase in Federal Medical Assistance – and a major condition of receiving that increase was a requirement to maintain continuous enrollment.
- When this condition ends, states will have up to 12 months to restart the normal enrollment process.
- This will include Medicaid, CHIP, and the Basic Health Program (BHP).
The Centers for Medicare & Medicaid Services (CMS) has established a tool for states to plan a return to the standard process for new and existing enrollees. States will be expected to submit data showing their completion of pending applications and reviewing renewals for those who are currently enrolled. CMS will be monitoring errors, timelines, and data submission by states and may require states to provide additional reporting on a more frequent basis.
Key Issues for States in the Toolkit to Ensure Compliance
- When the PHE ends, states will again renew eligibility requirements every 12 months for individuals enrolled in Medicaid and CHIP based on eligibility criteria. For individuals no longer eligible for the program they are enrolled in, states must consider other insurance affordability programs prior to terminating Medicaid and CHIP coverage.
- Applications must be handled promptly and may not exceed 90 days for a Medicaid applicant on the basis of disability, or 45 days for all others.
- States are encouraged to plan to comply with these requirements by considering staffing and organizational needs, prioritizing work, and determining mitigation strategies.
- The first step is to assess the processing of renewals to conduct post-enrollment verification and redeterminations of eligibility due to changes in the enrollee circumstances. While states will be required to initiate renewals for all individuals enrolled within 12 months, the month it begins may vary by state. States will have to evaluate the number of renewals, length of time pending, which populations may be stable (children, dually eligible individuals); populations that are vulnerable and other populations.
- Application processing is expected to be timely—CMS expects states to expeditiously process applications beginning immediately. States may use a phased-in approach to complete applications, such as two months after the month in which the PHE ends. States should complete eligibility determinations for those age 65 and older; three months after PHE ends, states should complete eligibility determinations for all pending disability-related applications; four months after the PHE ends, states should resume timely processing of all applications.
- CMS expects states will begin processing fair hearing requests timely after the PHE ends. The approach should be customized by each state depending on the volume, types of requests, and staffing.
- States should develop an outreach and communications plan, and in doing so, should consider the core audiences and key messages.
- States should have a month-to-month plan for completing eligibility determinations; timely application processing; initiating renewals by 12 months after the state begins its unwinding period; and completing all pending actions. This will require a detailed effort to communicate with existing populations of eligible individuals as well as those who have been covered previously.
CMS has identified additional guidance and resources for states in this transition to ensure a review of individuals enrolled in Medicaid and CHIP and assist them through the 12 month cycle with planning tools. Plans, providers, and other health care entities should monitor each state’s efforts carefully and assist in providing accurate information on the potential changes in coverage that may occur during this transition.
Clipped from: https://www.natlawreview.com/article/public-health-emergency-guidance-released-medicaid-and-children-s-health-insurance