
Helping you consider differing viewpoints. Before it’s illegal.
Article 1:
Behavioral health workforce faces critical challenges in meeting population needs, Elsevier, May 2018
Clay’s summary: This one has a map. Everybody loves a map!
Key Passage from the Article
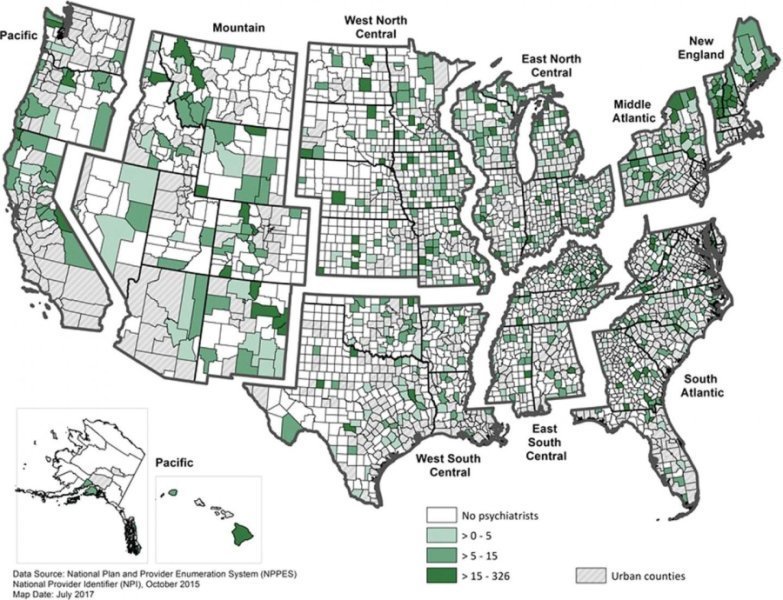
A 2016 report by the Health Resources and Services Administration (HRSA) on the projected supply and demand for behavioral health practitioners through 2025 indicated significant shortages of psychiatrists, psychologists, social workers, mental health counselors, and marriage and family therapists. The magnitude of provider shortages, however, is not the only issue when considering access to behavioral health services. Another major concern is maldistribution, since parts of the US have few or no behavioral health providers available, and access to mental health services is especially critical in areas of poverty.
“It is imperative that a plan be developed to address the resource limitations inhibiting the delivery of behavioral health services,” says Angela J. Beck, PhD, MPH, of the University of Michigan School of Public Health, Behavioral Health Workforce Research Center, Ann Arbor, MI, USA, one of the supplement’s Guest Editors. “This set of articles collectively proposes strategies and best practices to guide success of the current and future behavioral health workforce.”
…
Article 2:
HEALTHCARE TRANSPORTATION ‘DISRUPTERS’ MAKE BIG DRIVE IN NEW JERSEY, Lilo Stanton, NJ Spotlight, July 13, 2018
Clay’s summary: Another transport vendor enters the competition to solve NEMT challenges.
Key Passage from the Article
Roundtrip, which said it transports hundreds of New Jersey residents every week, also enables individuals anywhere in the state to book medical transportation for themselves, to any provider — by phone, through its website, or via free mobile apps. People can also use the system to arrange a ride for friends or family, regardless of where the patients live or the doctor’s location.
Founded in 2016, Roundtrip is now operating in more than 15 states, including New Jersey, and officials said business has tripled since January. The company wants to make it easier for people to access medical care, reduce the number of missed appointments and improve clinical outcomes — changes that can also reduce the cost of care. It can be particularly useful for patients who need regular and potentially debilitating treatments, like chemotherapy and dialysis, and helps hospitals free up beds when someone is ready to be discharged but lacks safe transportation to get home.
Article 3:
Long-term nursing care turnover linked to low Medicaid payments
Clay’s summary: The answer is clearly more money. Done! What complex problem is next? Bet we can fix that one with more money, too!
Key Passage from the Article
A study by the Texas Health Care Association, a nonprofit trade group representing nursing homes, says the annual turnover rate for certified nursing assistants is 97 percent. The churn rate for registered nurses and licensed vocational nurses is almost as high, coming in at 90 percent, according to a THCA study released this year. Kevin Warren, president and CEO of Austin-based THCA, said one of the primary issues is the state’s low Medicaid reimbursement rate of $143.48 per day. Only South Dakota provides a lower payment at $133.74. “When you look across the state, roughly two-thirds of the residents that reside in nursing facilities in the state, their care is paid for through Medicaid,” he said. “And we see that today’s Medicaid rate in skilled nursing is roughly about $27 a day less than what the cost of care is to deliver.” There are about three dozen long-term care facilities located in the Rio Grande Valley. Statewide, there are about 1,200 such facilities and they are caring for 90,000 residents. Warren said the low Texas Medicaid reimbursement means a long-term care facility is only paid about $6 per hour per patient for care, which hampers a nursing home company’s ability to compensate and retain nurses.
