MM Curator summary
[MM Curator Summary]: MH services provided by interns will now need to be supervised by licensed counselors with at least 2 years licensed experience and who are not barred from the program. And providers are up in arms about this.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
New rules about the supervision of counselors working toward their licenses could worsen the workforce shortage, private practice therapists say
Carla D’Agostino-Vigil, clinical director at Ignite Counseling Colorado, speaks during an employee meeting Feb. 23, 2022, in Westminister. D’Agostino-Vigil is one of Colorado’s mental health providers who has grown frustrated with billing issues with the state Medicaid program. (Hugh Carey, The Colorado Sun)
Colorado mental health counselors in private practice say they’ve been surprised once again with new rules that will make it harder to treat the state’s most vulnerable patients: those with Medicaid insurance.
The latest friction between behavioral health professionals and the Colorado Department of Health Care Policy and Financing centers on the supervision of post-graduate counselors working toward their state license.
The department — which approved the policy written by the regional agencies that handle payments to mental health clinics — says the new rules are necessary to ensure Medicaid patients are receiving quality care. But counselors in private practice say the rules could mean the loss of dozens of workers and potentially hundreds of mental health appointments.
They’re also frustrated because they said they didn’t know the new rules were coming.
The policy, which was announced at the beginning of this month, imposes stricter requirements on using interns still working toward their graduate degrees and therapists who have graduated but have yet to receive their license, a process that takes two to four years after graduation. Those pre-licensed counselors can see patients, but must have a licensed counselor sign off on their diagnoses and progress notes from each counseling session.
With the new rules, only counselors who have been licensed for at least two years can sign off on the work of pre-licensed counselors. The rules also stipulate that any counselor sanctioned by the state licensing division, at the Department of Regulatory Agencies, must wait for two years after their sanctions have expired before supervising pre-licensed counselors.
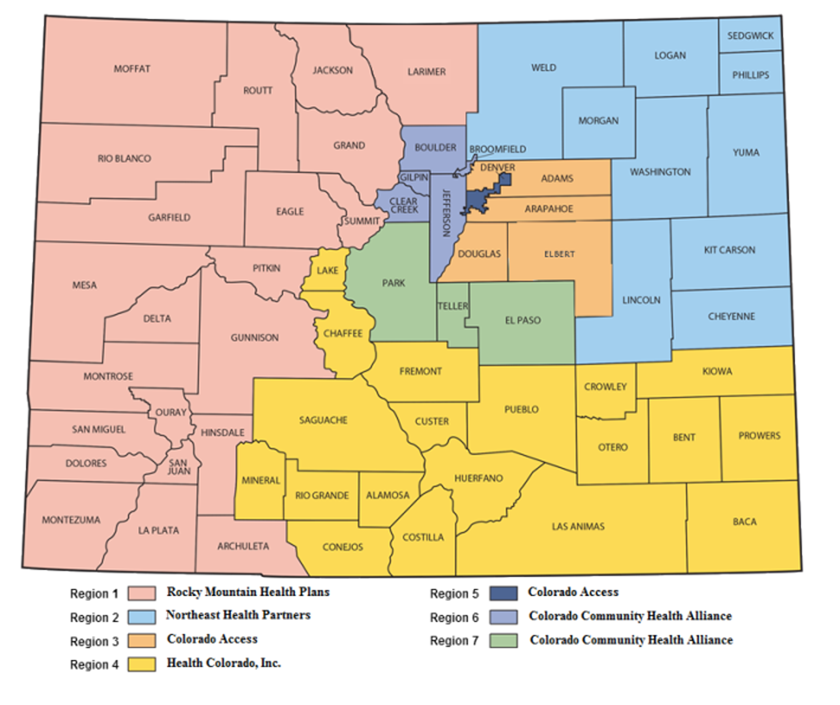
Colorado is divided into seven regions run by agencies that contract with the state Medicaid division. Behavioral health providers who want to take patients on Medicaid must enroll first at the state department and then with the regional agencies. (Colorado Department of Health Care Policy and Financing)
Counselors in private practice see both rules as an overreach, one that will mean fewer appointments for patients on the government insurance program for the needy, Medicaid. About 30 of them attended a virtual meeting this week with the Medicaid division, which is housed in the Department of Health Care Policy and Financing.
“We feel like that is going too far,” Andrew Rose, a psychotherapist and director of Boulder Emotional Wellness, said in an interview. “If DORA has decided you are safe to practice, that should be good enough.”
But Cristen Bates, the state’s interim Medicaid director, said the policy is geared toward expanding the workforce — by creating standardized rules so that counselors still seeking their license have a clear path to getting experience and becoming licensed counselors. The issue is that the regional agencies that serve as the middlemen between clinics and the state Medicaid department have had inconsistent rules as they’ve allowed pre-licensed counselors to practice under supervision. The new policy, which also applies to community mental health centers, was created by those agencies to apply to counselors statewide.
“We have to make sure that our members are getting high-quality care,” Bates said. “We were glad to see some very clear rules about when this is and is not appropriate.”
Where the department erred, Bates said, was in not informing behavioral health care professionals about the policy changes or showing them a draft ahead of the implementation date.
“The rollout was where we kind of had some challenges,” she said.
The regional agencies are now considering possible changes to the policy and have said they will not deny claims or penalize clinics that are not following the new rules. After the outcry from providers, the regional agencies backtracked on the July 1 implementation date. One of them, Colorado Access, said in an email to The Sun that the policy change is not in effect and that “any changes to our current program will include additional input and advance notice.”
Recommended
Medicaid payment issues plague host of Colorado caregivers and therapists who see low-income and disabled patients
The discord is the latest in a long list of frustrations among mental health professionals who say they want to provide therapy for people on Medicaid but are fed up dealing with burdensome rules, redundant paperwork and even threats of having payments revoked. It comes as Colorado is facing unprecedented need for services, due in part to the isolation and stress of the coronavirus pandemic.
Rose said he typically signs off on 100 to 200 notes per week for his team of pre-licensed staff at Boulder Emotional Wellness. The clinic employs 38 pre-licensed counselors and plans to bump that number to 42 next month.
The rule changes will make this a challenge, since it’s already difficult to find licensed counselors willing to take on the liability of supervising pre-licensed therapists, he said.
Recommended
Colorado’s new mental health commissioner to focus on “front-door” access to care, children and the fentanyl crisis
Rose and others said they found out about the policy in a July 5 newsletter from one of the regional agencies that also laid out other policies that went into effect July 1.
“The larger concern here is really, who sets policy and who gets to have a say in that process?” he said. “It’s hard enough right now to keep providers. We just need some relief from this. We need to be included in decisions about who we can hire.”
The need for mental health counseling is so high right now that appointments with licensed counselors are “filled in a hot second,” said Dr. Lisa Griffiths, director of the Center for Valued Living in Aurora. Many clients rely on appointments with pre-licensed counselors under the supervision of licensed counselors.
One of Griffiths’ seven supervisors has a doctoral degree but has not yet had her license for two years, meaning she could no longer supervise other counselors under the new rules.
Mental health providers have been meeting regularly with the Medicaid department to smooth out their relationship after a series of issues, including rate cuts and processing problems that resulted in a regional agency trying to take back money from clinics that had already been paid for seeing Medicaid clients.
In the past few months, providers and the department have collaborated on new policies for marriage therapists and treating patients with gender dysphoria. The latest policy changes, however, came out of nowhere, Griffiths said.
“The providers felt blindsided,” she said.
We believe vital information needs to be seen by the people impacted, whether it’s a public health crisis, investigative reporting or keeping lawmakers accountable. This reporting depends on support from readers like you.
Clipped from: https://coloradosun.com/2022/07/14/mental-health-medicaid-counselors/
