This post is only available to members. You register for FREE here or login if you are already a member
Category: Uncategorized
What are the key legislative committees and offices?
Who are the key members of the Governor’s cabinet for health and human services?
Recent legislation
Where can I find state budget information?
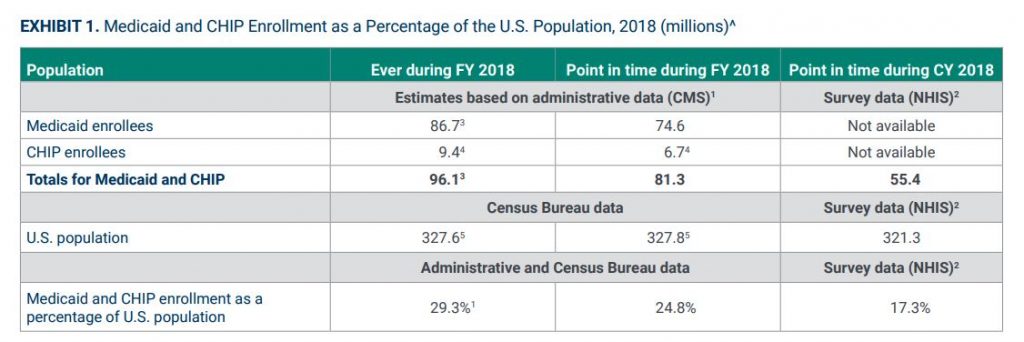
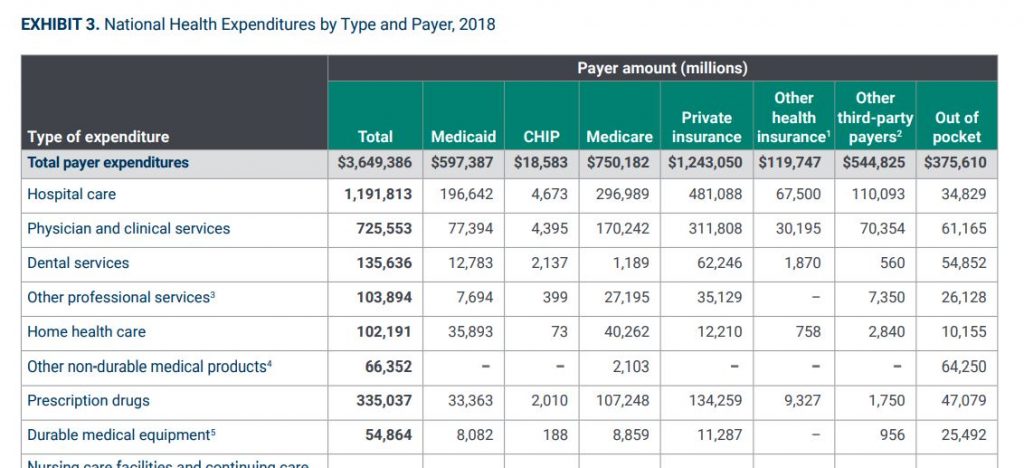
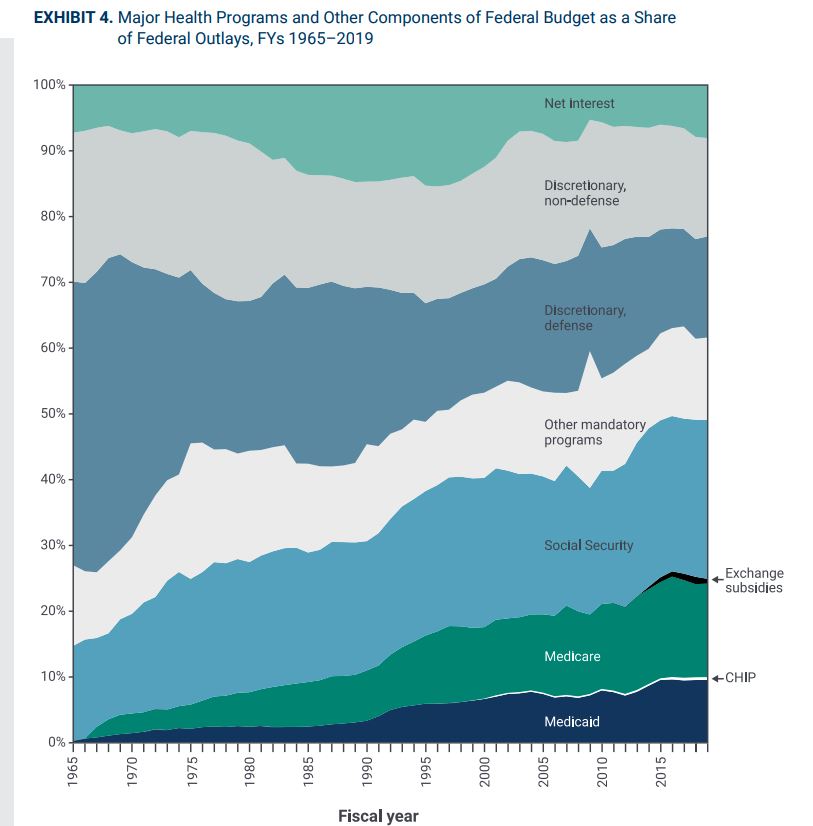
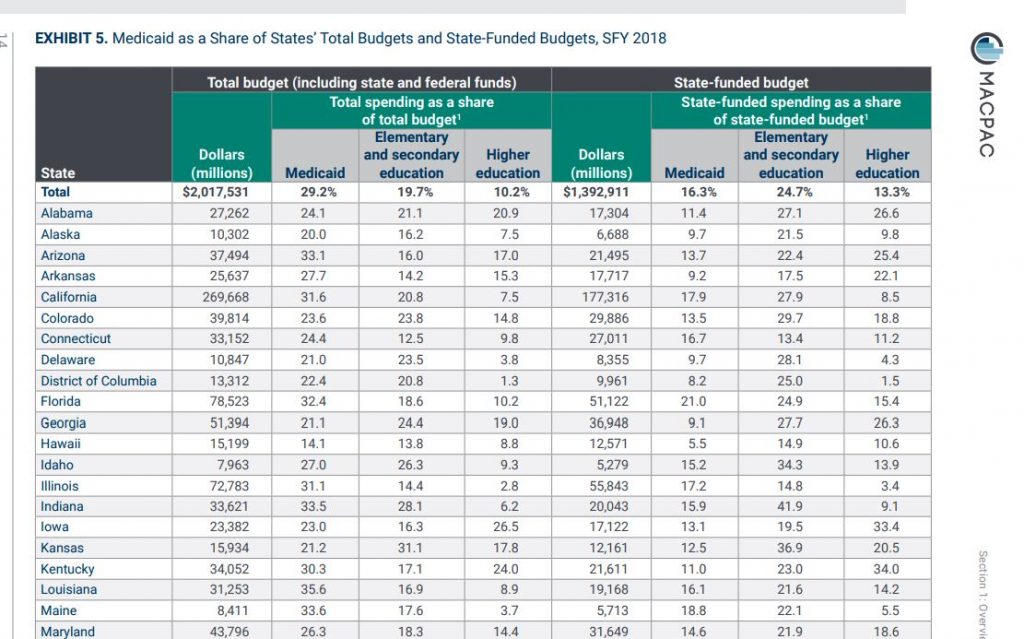
Data Set Review- 2020 MACStats Data Book

Summary
While MACPA puts out a Medicaid and CHIP data book each year, this one is especially important because it is the first one to use the T-MSIS data. If you watch Macpac.gov throughout the year, you will have seen much of the components of this compilation.
What’s in it
166 pages of charts and key statistics about all aspects of the Medicaid and CHIP programs, including data on:
- Enrollment (including demographics trends)
- Spending (health services and administrative)
- Eligibility levels by state
- Utilization
A detailed explanation of methodology used by the research team, including specifics on:
- The use of the T-MSIS data
- Adjustments for spending data
- A section on understanding managed care enrollment and spending data
Data sources included
National Health Interview Survey (NHIS)
The National Health Interview Survey (NHIS) has monitored the health of the nation since 1957. NHIS data on a broad range of health topics are collected through personal household interviews. Survey results have been instrumental in providing data to track health status, health care access, and progress toward achieving national health objectives.
The Medical Expenditure Panel Survey (MEPS)
The Medical Expenditure Panel Survey (MEPS) is a set of large-scale surveys of families and individuals, their medical providers, and employers across the United States. MEPS is the most complete source of data on the cost and use of health care and health insurance coverage.
Transformed Medicaid Statistical Information System (T-MSIS)
The T-MSIS data set contains:
- Enhanced information about beneficiary eligibility
- Beneficiary and provider enrollment
- Service utilization
- Claims and managed care data
- Expenditure data for Medicaid and CHIP
Key implications of this data set
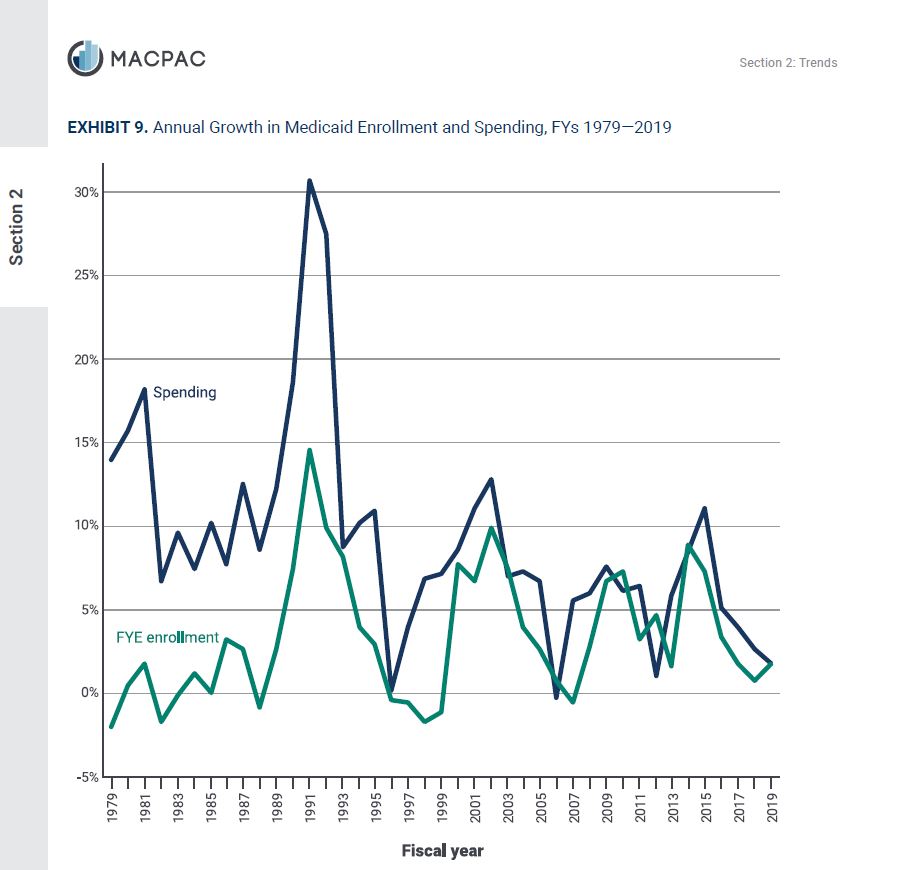
The trends section allows for some macro observations:
- The percent of Aged, blind or disabled members of the program was 28% in 1975. In 2018 it was 18%- giving credibility to the argument that the Medicaid program has experienced significant mission drift over the past 40 years or so.
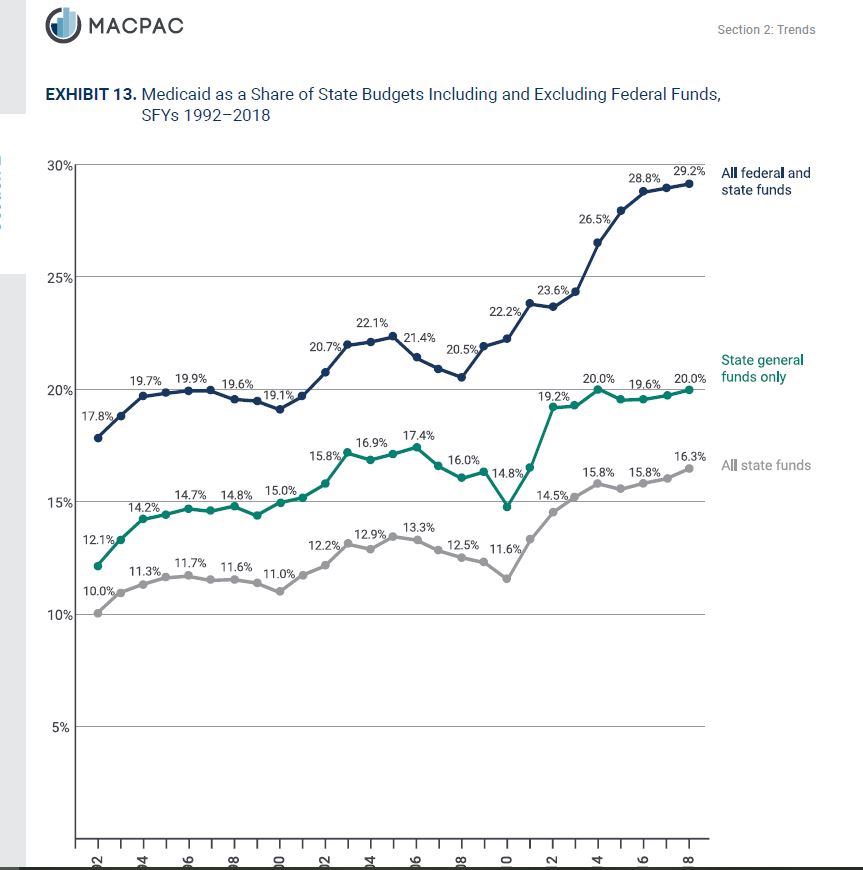
- The financial burden of Medicaid on states has doubled in the past twenty years, despite unprecedented levels of federal funding under the Affordable Care Act enhanced reimbursement for Medicaid expansion. In 1992, states spent 10% of their own money on Medicaid (as a percent of their entire state budget). In other words, 1 out of every 10 state dollars went to Medicaid. In 2018, it was 20%. Meaning 1 out of every 5 state dollars now must be spent on Medicaid.
- While trending data is not provided, it is interesting to see the percentages of Medicaid funds spent by benefit type. In descending order:
- Fee for service / direct payments
- Facilities – 22.5%
- Hospitals (13%)
- LTSS (“nursing homes”)- Institutional (9.5%)
- Clinics and health centers (2%)
- Providers – 14%
- Physicians (1.3%)
- Dentists (0.007%)
- Other practitioners (0.003%)
- LTSS- Home and Community Based (13%)
- Other acute services (7%)
- Drugs (0.008%)
- Facilities – 22.5%
- Managed Care – 50%
- Medicare Premiums – 3%
- Fee for service / direct payments
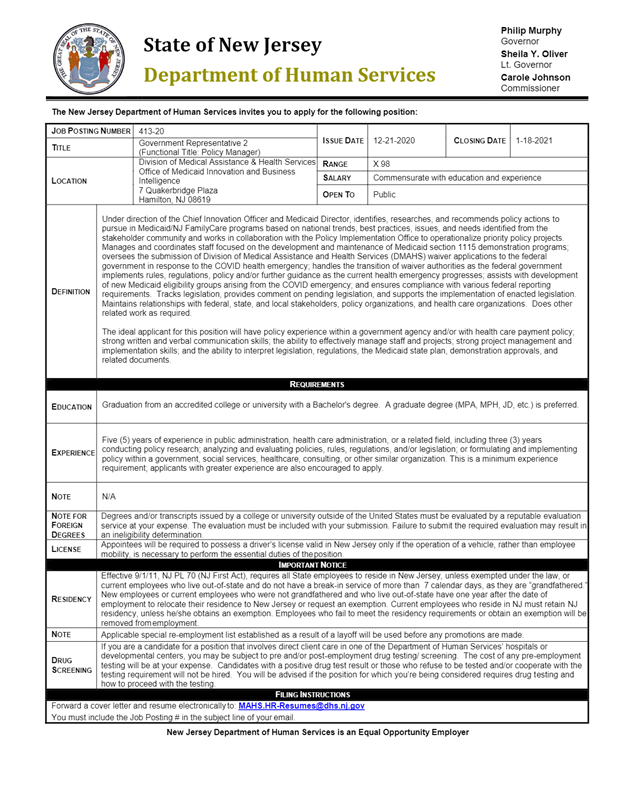
Policy Manager – New Jersey DHS
Deputy for Data Acquisition and Management- State of Washington Job Opportunities
|
|
|
Pharmaceutical Operations Manager
Long-Term Care Pharmacy Provider in Flint, MI is seeking Pharmaceutical Operations Manager: MBA; 36 months experience as pharmacy business manager. Salary $52,021/year.
- Assists CEO in development and implementation of both short and long-term plans, identify critical issues/opportunities by reviewing sales/financial analyses (i.e. cost/benefit analysis, data process modeling), utilize statistical techniques, use predictive modeling to devise practical solutions
- Develop approach to analyzing effectiveness of key processes and conduct impact assessment
- Conduct external research for improving efficiency of business operations using SWOT, PESTEL, 5 C analysis
- Assess process strengths and weaknesses, analytical procedures, transaction testing, bench marking of best practices across the business
- Assess new business opportunities; their potential impact, formulate strategic recommendations
- Define risk mitigation action plans to resolve process gaps.
- Analyzing the company’s position in the market, conduct detailed research analysis on competitors, analyzing growth and seasonal trends to predict demand.
- Oversee the marketing team in making and executing communication plans for both pharmacy team and nursing home e.g. setting up Quick Marr software.
- Analyze long term care facility needs, perceptions, and behavior through a combination of proprietary and syndicated customer research studies.
- Review and approve support documentation, work plans, and other deliverables by
- Defining the Swaps for the long-term facilities
- Managing the calendar for appropriate supply of medications to the nursing home care to minimize the inconvenience
- Synchronizing Long-term care facilities patient medications in order to deliver them on the same day, on a monthly basis by doing Medicine synchronization
- Switching of software to an upgraded version if needed and also supervise any technological advancement
- Update SOP’s for routine business operations
- Operations cost reduction by frequently providing managerial advice to enhance business, with the end desire to increase profits.
- Manage the coordination and performance of periodic physical inventories.
- Supervise department heads to allocate limited resources, efficient packaging schedules, managing the supply chain, and establish a competitive price structure.
- Supervise inventory management with the review of drug margins, ensure proper cost of goods sold is reported and make corrections for those drugs that show less than optimal margins.
- Supervise billing staff to ensure payment from insurance companies for 30,000 + claims per month through 835 upload or third-party checker (In-mar Reconciliation).
- Monitor over 60-day claims to ensure payment to reduce net aging cost for business.
- Manage the purchasing of pharmaceuticals process and buying team.
- Ensure proper research is performed to purchase the best product in terms of access, availability, supplier, price, and type of drug
- Ensuring proper minimum and maximum drug ordering limits are reviewed and maintained on a regular basis
- Monitor RX inventory levels and program efficiencies for Health and Wellness business units,
- Discontinuities of a product which is imminent due to drug back orders
- Monitor drug recalls and ensure compliance with drug supply chain security act (DSCSA)
- Minimize or eliminate DIR (Direct and Indirect Remuneration) fee by Medicaid, Blue Cross etc. to increase ASRX ratings to 5-star.
- Monitor compliance with supplier contract provisions.
- Coordinate nursing home and medical facilities client assignments, assure engagement efficiency and quality
- Maintain or develop vendor relationships. (i.e. Specialty RX items, OTC items, new/generic drug launches, flu vaccines) for inventory management.
- Act as the main point of contact for audits related to pharmacy inventory functions, billing, and ordering.
Clipped from: https://apply.recruitology.com/job/Zl8cNPzzC2HyTiSU8WDAp4agry8cSi/?cid=58168425
Contract Specialist (CMS)
Department of Health And Human Services
Office of Acquisition & Grants Management (OAGM)
- Videos

Duties
Summary
This position is located in the Department of Health & Human Services (HHS), Centers for Medicare & Medicaid Services (CMS), Office of Acquisition and Grants Management (OAGM).
As a Contract Specialist, GS-1102-11/12, you will be responsible for pre-award and post-award functions including price/cost analysis, negotiation, and administration for services for one or more organizations within Health & Human Services (HHS).
Responsibilities
- Develop strategic plans in conjunction with program officials and Contracting Officer’s Representatives (CORs).
- Prepare solicitation documents which incorporate required Federal Acquisition Regulations (FAR) and HHS policies and provisions.
- Perform cost/price analysis, including analysis of cost breakdowns to determine reasonableness and conformance to applicable regulations, directives, and policies.
- Prepare close-out documents to close contracts.
- Negotiate and prepare documents for contract modifications.
- This is a developmental position leading to the full performance duties listed above. The primary difference between the grade levels is in the areas of supervisory control and level of responsibility.
Travel Required
Not required
Supervisory status
No
Promotion Potential
12
- Job family (Series)
Requirements
Conditions of Employment
- You must be a U.S. Citizen or National to apply for this position.
- You will be subject to a background and suitability investigation.
Qualifications
ALL QUALIFICATION REQUIREMENTS MUST BE MET BY THE CLOSING DATE OF THIS ANNOUNCEMENT.
In order to qualify for the GS-11, you must meet the following: You must demonstrate in your resume at least one year (52 weeks) of qualifying specialized experience equivalent to the GS-09 grade level in the Federal government, obtained in either the private or public sector, to include: 1) Preparing acquisition documents and/or reports (examples: solicitations/contracts, market research, justifications & determinations, audit reports, negotiation objectives, or award documents); AND 2) Reviewing acquisition documents to ensure adherence to terms and conditions or regulations.
– OR –
Substitution of Education for Experience: You may substitute education for specialized experience at the GS-11 level by possessing a Ph.D. or equivalent doctoral degree, or 3 full years of progressively higher level graduate education leading to such a degree. Qualifying graduate education must be in one or a combination of the following fields: accounting, business, finance, law, contracts, purchasing, economics, industrial management, marketing, quantitative methods, or organization and management.
– OR –
Combination of Experience and Education: Only graduate education in excess of the amount required for the GS-09 grade level may be used to qualify applicants for positions at grades GS-11. Therefore, only education in excess of a master’s or equivalent graduate degree or 2 full years of progressively higher level graduate education leading to such a degree, may be used to combine education and experience.
TRANSCRIPTS are required to verify satisfactory completion of the educational requirement related to substitution of education for experience and combination of experience and education. Please see “Required Documents” section below for what documentation is required at the time of application.
In order to qualify for the GS-12, you must meet the following: You must demonstrate in your resume at least one year (52 weeks) of qualifying specialized experience equivalent to the GS-11 grade level in the Federal government, obtained in either the private or public sector, to include: 1) Gathering and analyzing information to draw conclusions about price/cost information; 2) Providing business-related advice, guidance or direction through communication; AND 3) Conducting negotiations on pricing, performance, compliance, or technical terms.
Substitution of Education for Experience: There is no substitution of education to meet the specialized experience requirement at the GS-12 grade level.
Combination of Experience and Education: There is no combination of experience and education to meet the specialized experience requirement at the GS-12 grade level.
Experience refers to paid and unpaid experience, including volunteer work done through National Service programs (e.g., Peace Corps, AmeriCorps) and other organizations (e.g., professional; philanthropic; religious; spiritual; community, student, social). Volunteer work helps build critical competencies, knowledge, and skills and can provide valuable training and experience that translates directly to paid employment. You will receive credit for all qualifying experience, including volunteer experience.
Education
Education Requirement: In addition to meeting the qualification requirements, all candidates must have the following educational requirements:
A. Possess a 4-year course of study leading to a bachelor’s degree with a major in any field from an accredited college or university. (Note: Unofficial or Official Transcripts must be submitted at the time of application.)
OR
B. Completed at least 24 semester hours in any combination of the following fields: accounting, business, finance, law, contracts, purchasing, economics, industrial management, marketing, quantitative methods, or organization and management. (Note: Unofficial or Official Transcripts must be submitted at the time of application.)
OR
C. On January 1, 2000, have held a position in the Federal service in the GS-1102 Contract Specialist series and I have continually held this occupational series since January 1, 2000. (Note: SF-50s must be submitted at the time of application.)
TRANSCRIPTS are required to verify satisfactory completion of the educational requirement listed above. Failure to submit a copy of your transcripts at the time of application WILL result in an ineligible rating. Please see “Required Documents” section below for what documentation is required at the time of application.
Click the following link to view the occupational questionnaire: https://apply.usastaffing.gov/ViewQuestionnaire/10995975
Additional information
Bargaining Unit Position: Yes
Tour of Duty: Flexible
Recruitment/Relocation Incentive: Not Authorized
Financial Disclosure: Not Required
CMS employees currently participating in 100% Full-Time Telework Program may be eligible to remain in the program. If an employee in this program is selected, the pay will be set in accordance with the locality pay for the applicable duty station. The listed salary range reflects the locality pay assigned to the duty location(s) listed in the vacancy announcement. For more information about pay based on locality, please visit the Office of Personnel Management (OPM) Salaries & Wages Page.
The Interagency Career Transition Assistance Plan (ICTAP) and Career Transition Assistance Plan (CTAP) provide eligible displaced federal employees with selection priority over other candidates for competitive service vacancies. To be qualified you must submit the required documentation and be rated well-qualified for this vacancy. Click here for a detailed description of the required supporting documents. A well-qualified applicant is one who meets the qualification standard and eligibility requirements for the position, including any medical qualifications (if applicable), minimal educational and experience requirements; meets all selective placement factors (if applicable); is physically qualified, with reasonable accommodation where appropriate, to perform the essential duties of the position; meets any special qualifying conditions that OPM has approved for the position; and is able to satisfactorily perform the duties of the position upon entry. Additional information about ICTAP and CTAP eligibility is on OPM’s Career Transition Resources website at www.opm.gov/rif/employee_guides/career_transition.asp.
Additional Forms REQUIRED Prior to Appointment:
- Optional Form 306, Declaration of Federal Employment and the Background/Suitability Investigation – A background and suitability investigation will be required for all selectees. Appointment will be subject to the successful completion of the investigation and favorable adjudication. Failure to successfully meet these requirements may be grounds for appropriate personnel action. In addition, if hired, a reinvestigation or supplemental investigation may be required at a later time. If selected, the Optional Form 306 will be required prior to final job offer. Click here to obtain a copy of the Optional Form 306.
- Form I-9, Employment Verification and the Electronic Eligibility Verification Program – CMS participates in the Electronic Employment Eligibility Verification Program (E-Verify). E-Verify helps employers determine employment eligibility of new hires and the validity of their Social Security numbers. If selected, the Form I-9 will be required at the time of in-processing. Click here for more information about E-Verify and to obtain a copy of the Form I-9.
- Standard Form 61, Appointment Affidavits – If selected, the Standard Form 61 will be required at the time of in-processing. Click here to obtain a copy of the Standard Form 61.
If you are unable to apply online or need to fax a document you do not have in electronic form, view the following link for information regarding an Alternate Application.
How You Will Be Evaluated
You will be evaluated for this job based on how well you meet the qualifications above.
Additional selections may be made for similar positions across the Department of Health and Human Services (HHS) within the local commuting area(s) of the location identified in this announcement. By applying, you agree to have your application shared with any interested selecting official(s) at HHS. Clearance of CTAP/ICTAP will be applied for similar positions across HHS.
Traditional rating and ranking of applications does not apply to this vacancy. Applications will be evaluated against the basic qualifications. Qualified candidates will be referred for consideration in accordance with the Office of Personnel Management direct hire guidelines. Veterans’ Preference does not apply to direct hire recruitment procedures. Selections made under this vacancy announcement will be processed as new appointments to the civil service. Current civil service employees would, therefore, be given new appointments to the civil service; however, benefits, time served and all other Federal entitlements would remain the same.
Background checks and security clearance
Security clearance
Drug test required
No
Position sensitivity and risk
Trust determination process
Credentialing, Suitability/Fitness
Required Documents
The following documents are REQUIRED:
1. Resume
showing relevant experience; cover letter optional. Your resume must indicate your citizenship and if you are registered for Selective Service if you are a male born after 12/31/59. Your resume must also list your work experience and education (if applicable) including the start and end dates (mm/dd/yy) of each employment along with the number of hours worked per week. For work in the Federal service, you must include the series and grade level for the position(s). Your resume will be used to validate your responses to the assessment tool(s). For resume and application tips visit: https://www.usajobs.gov/Help/faq/application/documents/resume/what-to-include/
2. CMS Required Documents (e.g., SF-50, DD-214, SF-15, etc.). Required documents may be necessary to be considered for this vacancy announcement. Click here for a detailed description of the required documents. Failure to provide the required documentation WILL result in an ineligible rating OR non-consideration.
3. College Transcripts. Since this position requires specific education, you must submit a transcript attesting to your possession of the required education. You may submit an unofficial transcript or a list of college courses completed indicating course titles, credit hours, and grades received. An official transcript is required if you are selected for the position. If selected, you must provide an original document before the final job offer may be extended. If you do not submit a transcript indicating your possession of the required education, you will not be considered for this position.
College Transcripts and Foreign Education: Applicants who have completed part or all of their education outside of the U.S. must have their foreign education evaluated by an accredited organization to ensure that the foreign education is comparable to education received in accredited educational institutions in the U.S. For a listing of services that can perform this evaluation, visit the National Association of Credential Evaluation Services website. This list, which may not be all inclusive, is for informational purposes only and does not imply any endorsement of any specific agency.
If you are applying for a position for which a state license is issued (e.g., physician, engineer, attorney) possession of a valid and current U.S. professional license by a graduate of a foreign professional school or program is sufficient proof that the foreign education has been determined to be equivalent to the requisite U.S. professional education in that occupational field.
PLEASE NOTE: A complete application package includes the online application, resume, transcripts and CMS required documents. Please carefully review the full job announcement to include the “Required Documents” and “How to Apply” sections. Failure to submit the online application, resume, transcripts and CMS required documents, will result in you not being considered for employment.
If you are relying on your education to meet qualification requirements:
Education must be accredited by an accrediting institution recognized by the U.S. Department of Education in order for it to be credited towards qualifications. Therefore, provide only the attendance and/or degrees from schools accredited by accrediting institutions recognized by the U.S. Department of Education.
Failure to provide all of the required information as stated in this vacancy announcement may result in an ineligible rating or may affect the overall rating.
Benefits
A career with the U.S. Government provides employees with a comprehensive benefits package. As a federal employee, you and your family will have access to a range of benefits that are designed to make your federal career very rewarding. Learn more about federal benefits.
Eligibility for benefits depends on the type of position you hold and whether your position is full-time, part-time, or intermittent. Contact the hiring agency for more information on the specific benefits offered.
How to Apply
Your complete application package, as described in the “Required Documents” section, must be received by 11:59 PM ET on 01/15/2021 to receive consideration.
IN DESCRIBING YOUR WORK EXPERIENCE AND/OR EDUCATION, PLEASE BE CLEAR AND SPECIFIC REGARDING YOUR EXPERIENCE OR EDUCATION.
We strongly encourage applicants to utilize the USAJOBS resume builder in the creation of resumes. Please ensure EACH work history includes ALL of the following information:
- Official Position Title (include series and grade if Federal job)
- Duties (be specific in describing your duties)
- Employer’s name and address
- Supervisor name and phone number
- Start and end dates including month, day and year (e.g. June 18, 2007 to April 05, 2008)
- Full-time or part-time status (include hours worked per week)
- Salary
Determining length of general or specialized experience is dependent on the above information and failure to provide ALL of this information WILL result in a finding of ineligible.
- To begin, click Apply to access the online application. You will need to be logged into your USAJOBS account to apply. If you do not have a USAJOBS account, you will need to create one before beginning the application.
- Follow the prompts to select your resume and/or other supporting documents to be included with your application package. You will have the opportunity to upload additional documents to include in your application before it is submitted. Your uploaded documents may take several hours to clear the virus scan process.
- After acknowledging you have reviewed your application package, complete the Include Personal Information section as you deem appropriate and click to continue with the application process.
- You will be taken to the online application which you must complete in order to apply for the position. Complete the online application, verify the required documentation is included with your application package, and submit the application.
To verify the status of your application, log into your USAJOBS account (https://my.usajobs.gov/Account/Login), all of your applications will appear on the Welcome screen. The Application Status will appear along with the date your application was last updated. For information on what each Application Status means, visit: https://www.usajobs.gov/Help/how-to/application/status/.
This agency provides reasonable accommodation to applicants with disabilities. If you need a reasonable accommodation for any part of the application or hiring process, please send an email to Sandy.Vises@cms.hhs.gov. The decision to grant reasonable accommodation will be made on a case-by-case basis.
Commissioned Corps Officers (including Commissioned Corps applicants that are professionally boarded) who are interested in applying for this position must send their professional resume (not PHS Curriculum Vitae) and cover letter to CMSCorpsJobs@cms.hhs.gov in lieu of applying through this announcement. The cover letter should specifically explain how you are qualified for this position and draw specific attention to your resume that demonstrates these qualifications. In the subject line of your e-mail please include only the Job Announcement Number. In the body of your e-mail please include your current rank name and serial number. Failure to provide this information may impact your consideration for this position.
Agency contact information
Sandy Vises
Email
Address
Office of Acquisition and Grants Management
7500 Security Blvd
Woodlawn, MD 21244
US
Next steps
Once your online application is submitted, you will receive a confirmation notification by email. Within 30 business days of the closing date,01/15/2021, you may check your status online by logging into your USAJOBS account (https://my.usajobs.gov/Account/Login). We will update your status after each key stage in the application process has been completed.
- Fair & Transparent
The Federal hiring process is setup to be fair and transparent. Please read the following guidance.
Equal Employment Opportunity Policy
The United States Government does not discriminate in employment on the basis of race, color, religion, sex (including pregnancy and gender identity), national origin, political affiliation, sexual orientation, marital status, disability, genetic information, age, membership in an employee organization, retaliation, parental status, military service, or other non-merit factor.
Reasonable Accommodation Policy
Federal agencies must provide reasonable accommodation to applicants with disabilities where appropriate. Applicants requiring reasonable accommodation for any part of the application process should follow the instructions in the job opportunity announcement. For any part of the remaining hiring process, applicants should contact the hiring agency directly. Determinations on requests for reasonable accommodation will be made on a case-by-case basis.
A reasonable accommodation is any change to a job, the work environment, or the way things are usually done that enables an individual with a disability to apply for a job, perform job duties or receive equal access to job benefits.
Under the Rehabilitation Act of 1973, federal agencies must provide reasonable accommodations when:
- An applicant with a disability needs an accommodation to have an equal opportunity to apply for a job.
- An employee with a disability needs an accommodation to perform the essential job duties or to gain access to the workplace.
- An employee with a disability needs an accommodation to receive equal access to benefits, such as details, training, and office-sponsored events.
You can request a reasonable accommodation at any time during the application or hiring process or while on the job. Requests are considered on a case-by-case basis.
Learn more about disability employment and reasonable accommodations or how to contact an agency.
Legal and regulatory guidance
- Financial suitability
- Social security number request
- Privacy Act
- Signature and false statements
- Selective Service
- New employee probationary period
Clipped from: https://www.usajobs.gov/GetJob/ViewDetails/588032300