





Curator, Managed Care, North Carolina
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
Curator summary
NC managed care now is required to move forward by the legislature by July 2021, though protests/ lawsuits are still pending.
Clipped from: https://www.northcarolinahealthnews.org/2020/09/29/medicaid-managed-care-companies-take-protest-to-court-again/
In the middle of a coronavirus pandemic that has tossed up challenge after challenge, the state Department of Health and Human Services also must tend to another enormous project.
Over the next 10 months, the department has been told by the legislature to complete the transformation of its cumbersome Medicaid system.
In the current system, the state pays for each office visit, test and hospitalization for the seniors and children enrolled in Medicaid. By July 1, North Carolina is expected to launch a managed-care system in which private insurance companies get lump-sum payments from the state to pay providers for their overall care of most of the state’s 2.3 million beneficiaries.
North Carolina lags behind the rest of the country in making this switch and the changeover has been touted by Republican legislators as a potential cost-saver for the state.
As DHHS staff tend to the details of the massive switch of how some 1.6 million Medicaid patients will get health care, companies that lost out on bids for a share of the more than $30 billion the state will dole out over the next five years are stepping up their challenges in court.
In late August, an administrative law judge ruled against Aetna, Optima and My Health By Health Providers, companies that argued DHHS unfairly awarded Blue Cross Blue Shield of North Carolina a contract.
My Health By Health Providers, a consortium of major hospital systems in North Carolina, petitioned a Wake County Superior Court judge this week to reverse that decision.
In the court document filed on Sept. 23, the provider-led entity, or PLE, argued that the contract awarding process gave a weighted bias to traditional insurance companies over the 12 health systems that have joined together as My Health By Health Providers.
They argue that their owners, which already serve more than 1 million Medicaid beneficiaries each year, are in a better position to provide the managed care, in part, because they are in North Carolina and familiar with the health needs already.
They are troubled that the judge issued a ruling in summary judgment, a step that precluded them from presenting their entire body of evidence in a hearing.
Lisa Farrell, executive director of My Health By Health Providers, said her organization was only before the administrative law judge for two hours of arguments.
On Monday, she ticked off a few reasons why she thought the DHHS process was rigged against PLEs from the start. She also explained why My Health By Health Providers is continuing its challenge in Wake County Superior Court instead of trying again when the procurement process opens again.
It’s best to be in on the ground-level, she said.
“One of the considerations as you go forward is members will establish themselves,” Farrell said.
Though My Health By Health Providers was the highest PLE scorer in the bidding process, the state argues that it was looking for a regional plan and the conglomeration of health care systems had pitched a statewide plan. The 2015 law mandating the Medicaid switchover stipulates that PLEs can bid for business in a region, or two contiguous regions, but doesn’t say anything about PLEs bidding for all of the state’s regions.
Farrell argues that My Health By Health Providers’ bid also offered regional options.
While explaining why she thinks PLEs are needed in North Carolina to complement and challenge the managed care that traditional insurance companies provide, Farrell gave an example of a pediatrician in rural North Carolina treating a child with a complex illness.
The health care systems comprising My Health By Health Providers include Atrium Health, Cape Fear Valley Health, CaroMont Health, Cone Health, Duke Health, Mission Health, New Hanover Regional Medical Center, Novant Health, UNC Health, Vidant Health, Wake Forest Baptist Health, and WakeMed Health and Hospitals, some of which are connected to academic research centers.
With that connection, the rural provider could get the patient quickly linked to a health care facility that could provide the more complex care, Farrell argued.
“Providers, because they are providing the care, are really closer to their beneficiaries,” Farrell said.
The state’s selections for the coveted managed-care contracts were announced in February 2019. The awards went to four well-established insurance companies: AmeriHealth Caritas, Blue Cross and Blue Shield of North Carolina, UnitedHealthcare and WellCare. Carolina Complete Health, a provider-led group that will be run by Centene, a managed care giant, was the sole provider-led entity selected. The N.C. Medical Society backed that plan.
In challenges that started last year in the state Office of Administrative Hearings, My Health By Health Providers, Aetna and Optima Health, another provider-led group linked to Virginia’s Sentara Healthcare, argued that DHHS employees involved in the contract awarding process had conflicts of interest that caused them to favor BCBSNC over their bids.
The state and BCBSNC have disputed those claims, and on Aug. 25, Tenisha Jacobs, an administrative law judge, sided with them, ruling that the contract had been properly awarded.
DHHS issued a statement several days after the decision.
“The NC Department of Health and Human Services (NCDHHS) is pleased to announce that once again court rulings affirm the integrity and fairness of the Departments’ managed care procurement process,” according to the statement.
Jacobs heralded the possibility of such an outcome in a June 2019 ruling before the companies had presented all their evidence. They had asked her to halt the Medicaid system transformation while their court cases remained unresolved.
Though Jacobs ruled against the request, saying the companies seemed unlikely to succeed on the merits of their claims, the transformation was instead put on hold in late 2019 because of a budget standoff between Gov. Roy Cooper and Republicans leading both General Assembly chambers.
The transformation had been scheduled to begin in February of this year, but the General Assembly closed its 2019 session without a budget that dedicated funding to the project.
This summer, the General Assembly set a new deadline. Lawmakers considered penalizing DHHS if the transformation did not occur by July 1, raising the possibility that the department could be charged millions of dollars for each month after that date that the launch did not occur.
Eventually, the bill that passed did not include penalties.
“North Carolina’s approach to managed care has received national recognition and focuses on improving the health of North Carolinians through an innovative, whole-person centered and well-coordinated system of care that addresses both the medical and non-medical drivers of health,” according to the DHHS statement issued in August after the ruling.
Aetna immediately appealed the August ruling in Wake County Superior Court.
“For the past 18 months, Aetna Better Health has dutifully followed the Office of Administrative Hearings’ (OAH) protest process in our protesting the North Carolina Department of Health and Human Services’ (DHHS) awarding of contracts for prepaid health services regarding the state’s Medicaid program on several grounds, including, but not limited to, conflicts of interest between DHHS and certain awarded carriers, changes in the scoring process by DHHS to benefit certain awarded carriers, and DHHS’ attempt to conceal how scores were changed to benefit particular awarded carriers,” Aetna said in a company statement at the time. “After a year and half of protest with little progress, we are left no viable choice procedurally but to pursue our Medicaid protests against DHHS in Superior Court.”
Dave Richard, deputy DHHS secretary for NC Medicaid, said in an interview last week that while he’s confident in the process used to award the contracts, legal challenges were not unusual.
“I think we’re seeing that across the country that that happens,” Richard said. “No one wants to go through this process. It takes time from people, but we were always prepared that this is a possibility.”
As part of the legal defense, the department produced some 230,000 pages of documents and staff members had to sit through weeks and weeks of depositions.
“The judge ruled in our favor,” Richard said. “We believed she ruled correctly, and we have no reason to believe that there’ll be anything different that happens in the appeal.”
The challengers hope for a different outcome, arguing that they did not get to present all their evidence to the administrative judge.
Matt Salo, executive director of the National Association of Medicaid Directors, said the challenges in North Carolina are not unique, but all that litigation eventually might lead states to reconsider managed care systems.
“I appreciate that this is really important stuff, that this is big business, these are contracts that are very, very meaningful,” Salo said in a telephone interview last week. “But having said that, if we keep going on this trajectory, where everybody who doesn’t like the outcome, just resorts to the courts, and sues and has a bid protest, we’re going to end up in a world where states are just going to throw their hands up and say, ‘You know what, it’s easier if we just go back to fee for service.'”
Salo did not speak specifically about the North Carolina cases, but acknowledged that some companies that lose out on contracts might have legitimate concerns that should be litigated.
In Louisiana, contracts worth billions of dollars were thrown out in January after the state’s chief procurement officer determined the health department had mishandled the bidding process.
Two losing bidders helped reveal the problems in challenges filed by Louisiana Healthcare Connections and Aetna Better Health, which banded together to complain of conflicts of interest, a skewed process and improprieties.
“There can be a role for a protest, you know, if something serious has gone wrong, if there was a serious mistake that was made, and sometimes that happens,” Salo said. “You know, it’s important to have an outlet. …There are legitimate protests. And if that’s the case, you should do it.
“What I’m worried about is the trend where it’s just, it’s just a knee jerk reaction of ‘I didn’t like the option. So, I’m escalating to the next step.'”

This edition of the 5 Slide Series tabulates new COVID tests, cases, and deaths per 100,000 population at a state level to examine how the COVID-19 pandemic has shifted September 1- 15 versus August 1 – 15. Nationally, trends have mostly moved in a favorable direction. During the first half of September relative to the first half of August, confirmed cases and deaths have decreased by more than 20%, and positive tests as a percent of all administered tests during each timeframe have decreased from 7.1% to 5.2%. However, several states have trended in an adverse direction and reported an increase in new cases, deaths, and positive tests September 1 – 15 versus August 1 – 15.


Today’s edition of the 5 Slide Series investigates recent COVID-19 death trends in the United States at both state and county levels. Nationally, the number of new COVID deaths decreased by 19% September 3 – 10 as compared to the previous week (August 27 – September 3). Despite this national decrease, five states (Hawaii, West Virginia, Arkansas, Montana, and Tennessee) reported that more than 15% of their cumulative COVID deaths occurred during the past two weeks. We also identified counties with more than 100,000 residents that reported the largest per capita death rates as of September 10 and over the past week.
5 Slide Series_Assessment of Recent State COVID Deaths_Sept 14




Today’s edition tracks recent COVID deaths in the USA in two ways. The national weekly progression has been tabulated across the past two months, showing a decrease of 6% this past week versus the previous week. However, new daily deaths remain near 1,000. We also show daily COVID deaths by state comparing June, July, and August. In 26 states across these months, the average number of daily deaths has been highest in August.

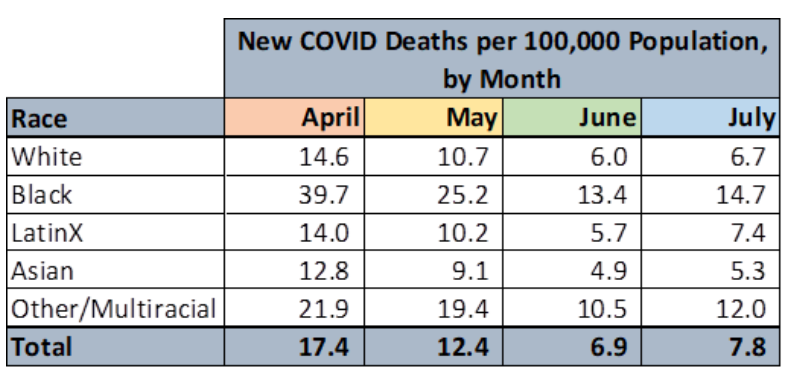
This week, we’ve revisited disparities in COVID deaths by race and by age cohort, showing monthly progressions during the pandemic. An excerpted table from this edition is pasted below. We’ve also assessed the proportion of all COVID deaths attributable to nursing home residents and how this has evolved over time.

Weekly and Monthly Progression of Deaths Attributed to COVID-19 8.6.20

Today’s edition of our 5 Slide Series is attached and frames how the USA’s COVID death rate compares with other highly developed countries (our death rate is 78% higher). We also portray each state’s weekly progression of COVID tests, cases, and deaths through the month of July. July has been a disappointing “step backwards” month in the USA overall and especially so in many states. Nationwide, we experienced nearly twice as many COVID deaths this past week as occurred during the first week of July.
Comparisons of COVID Death Rates Across Countries and States, July 31 2020

The Menges Group puts out these great analyses and insights each month. And is kind enough to let us repost them for the MM audience. Check out themengesgroup.com to learn more about the work they do.
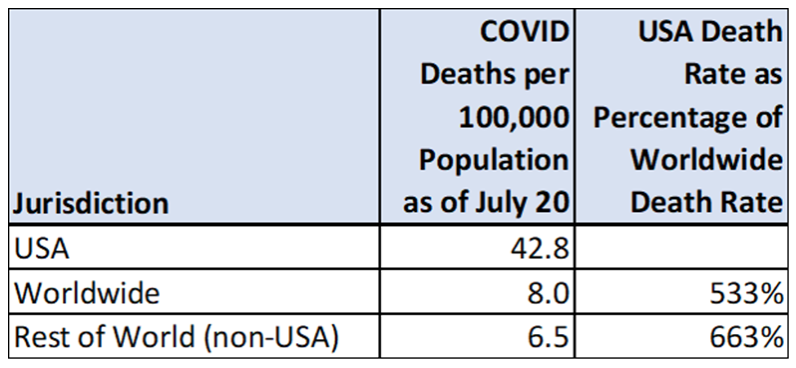
This week’s edition of our 5 Slide Series assesses the COVID death rate in the United States in a global context. The cumulative COVID death rate in the USA to date is 6.6 times higher than the rest of the world’s collective rate. Of the 160 countries whose COVID death rates have been tracked by Johns Hopkins University, the USA’s rate is 10th highest. One of this edition’s summary tables is shown below.
This edition also speaks to the need for accurate and objective data dissemination to optimally address the pandemic.