Helping you consider differing viewpoints. Before it’s illegal.
Article 1:
Details of federal health care fraud probe show how massive the problem is, Bethany Blankley, The Hayride, July 24th, 2018
Clay’s summary: 601 defendants. $2B stolen. All from your paycheck. Work hard!
Key Passage from the Article
Less than a month after the largest federal health care fraud sting in American history, details of the operation show how massive the problem is. As part of the operation, more than 600 people were charged with committing more than $2 billion in fraud and taxpayer theft. “Health care fraud is a betrayal of vulnerable patients, and often it is theft from the taxpayer,” Attorney General Jeff Sessions said. “In many cases, doctors, nurses, and pharmacists take advantage of people suffering from drug addiction in order to line their pockets. These are despicable crimes.” The investigation was led by the Department of Justice (DOJ) and the Department of Health and Human Services (HHS). The joint action involved more than 1,000 federal, state, local, and tribal law enforcement officers. The 601 defendants include 165 doctors, nurses, pharmacists, and medical professionals in 29 states and the District of Columbia, who are accused of financially profiting from more than $2 billion in false health care billings. In addition to criminal charges, HHS announced that 2,700 individuals were excluded from government health care programs since July 2017. The multi-agency investigation targeted fraudulent schemes that billed Medicare, Medicaid, TRICARE (a health insurance program for U.S. military members, their families, and veterans), and private insurance companies for “medically unnecessary” services or services that were never rendered. Bills were submitted for payment for prescription drugs and compounded medications that were rarely or never purchased or distributed to beneficiaries. Some doctors and medical professionals also distributed opioids and other prescription narcotics unlawfully, according to DOJ.
…
Read it here
Article 2:
CMS Needs to Better Target Risks to Improve Oversight of Expenditures, GAO, August 6th, 2018
Clay’s summary: No one really cares. Just keep the money flowing or else we will call you bad names.
Key Passage from the Article
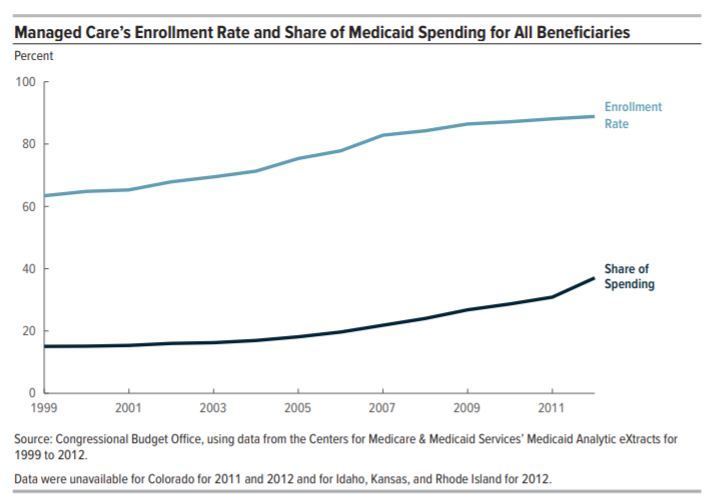
What GAO Found
The Centers for Medicare & Medicaid Services (CMS), which oversees Medicaid, has various review processes in place to assure that expenditures reported by states are supported and consistent with Medicaid requirements. The agency also has processes to review that the correct federal matching rates were applied to expenditures receiving a higher than standard federal matching rate, which can include certain types of services and populations. These processes collectively have had a considerable federal financial benefit, with CMS resolving errors that reduced federal spending by over $5.1 billion in fiscal years 2014 through 2017.
However, GAO identified weaknesses in how CMS targets its resources to address risks when reviewing whether expenditures are supported and consistent with requirements. CMS devotes similar levels of staff resources to review expenditures despite differing levels of risk across states. For example, the number of staff reviewing California’s expenditures—which represent 15 percent of federal Medicaid spending—is similar to the number reviewing Arkansas’ expenditures, which represents 1 percent of federal Medicaid spending. CMS cancelled in-depth financial management reviews in 17 out of 51 instances over the last 5 years. These reviews target expenditures considered by CMS to be at risk of not meeting program requirements. CMS told GAO that resource constraints contributed to both weaknesses. However, the agency has not completed a comprehensive assessment of risk to (1) determine whether oversight resources are adequate and (2) focus on the most significant areas of risk. Absent such an assessment, CMS is missing an opportunity to identify errors in reported expenditures that could result in substantial savings to the Medicaid program.
GAO also found limitations in CMS’s processes for reviewing expenditures that receive a higher federal matching rate. Internal guidance for examining variances in these expenditures was unclear, and not all reviewers in the three CMS regional offices GAO reviewed were investigating significant variances in quarter-to-quarter expenditures. Review procedures for expenditures for individuals newly eligible for Medicaid under the Patient Protection and Affordable Care Act were not tailored to different risk levels among states. For example, in its reviews of a sample of claims for this population, CMS reviewed claims for the same number of enrollees—30—in California as for Arkansas, even though California had 10 times the number of newly eligible enrollees as Arkansas. Without clear internal guidance and better targeting of risks in its review procedures for expenditures receiving higher matching rates, CMS may overpay states.
Read it here
Article 3:
Research: Medicaid expansion serves as employment incentive for people with disabilities, Tim Carpenter, The Garden City Telegram, July 24, 2018
Correcting an injustice: HHS moves to stop unions from skimming from Medicaid, Chantal Lovell & Vincent Vernuccio, Washington Examiner, August 07, 2018
Clay’s summary: So more healthcare means people will be healthier to work? And its also evil to expect them to do so if they can? I’m confused…
Key Passage from the Article
Research involving the University of Kansas and partner organizations showed individuals who reported not working because of a disability declined in Medicaid expansion states. In 2013, data showed 41.3 percent of individuals with disabilities in expansion states were employed or self-employed. That number escalated to 47 percent in 2017. In the same period, the percentage of the population that reported not working because of disability dropped from 32 percent to 27 percent. Those trends weren’t present in non-expansion states. In effect, the KU Institute for Health and Disability Policy Studies viewed Medicaid expansion as an employment incentive for people with disabilities.
“The takeaway is that, over time, these changes are becoming more robust,” said Jean Hall, professor of applied behavioral science and director of the KU institute. “Our argument is that, over time, those who are better able to manage their health would have a better ability to be employed.” Thirty-two states and the District of Columbia have expanded Medicaid eligibility under a law obligating the federal government to pay no less than 90 percent of the cost of expanded services. In the five-state region that includes Kansas, only Colorado has expanded. Nebraska, Oklahoma, Missouri and Kansas have not. Colyer, who took over for Brownback in January and is seeking the GOP nomination for governor in the Aug. 7 primary, said he supported work requirements within the state’s Medicaid system and opposed expansion of eligibility for Medicaid coverage under the 2010 federal law.
“I’ve been fighting Obamacare and its skyrocketing premiums with shrinking benefits since before it passed,” Colyer said. “Medicaid expansion is not financially sustainable and it focuses on the wrong people.” Sheldon Weisgrau, with the pro-Medicaid expansion group Alliance for a Healthy Kansas, said research showed Ohio’s expanded system improved the health of participants so they could be part of the workforce. “The main reason people on Medicaid don’t work is they’re not healthy enough to work,” said Weisgrau, who disputed the idea expanded Medicaid was unsustainable. “In fact, it is helping the state budgets of most of the states that are participating.”..
Read it here