MM Curator summary
A group of TN doctors got paid by Medicare and TN Medicaid for an implantable acupuncture device that was not covered.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
The exterior of the United States Department of Justice on Feb 16, 2018 in Washington, D.C.
ALEX EDELMAN/AFP/Getty Images
NASHVILLE (WSMV) – Don Cochran, U.S. Attorney for the Middle District of Tennessee, and Herbert Slatery III, Attorney General for the State of Tennessee, announced today that they have settled claims between three providers for false liability under the False Claims Act for the alleged improper billing for electro-acupuncture using a peri-auricular stimulation device known as “P-Stim” that does not qualify for reimbursement under Medicare or TennCare.
James P. Anderson, M.D. (“Dr. Anderson”), owner of Affiliated Neurologists, PLC; Charles F. Spencer, D.C., owner of Total Family Physicians Center PLLC d/b/a Total Family Health & Wellness (“Total Family”); and Mitchell P. Shea, D.C., owner of Chiro2Med of Tennessee P.C. (“Chiro2Med”) agreed to pay a combined $1.72 million to resolve liability.
P-Stim is an electro-acupuncture device that, pursuant to manufacturer’s instructions, is affixed behind a patient’s ear using an adhesive.
Once activated, the device then provides intermittent stimulation by electrical pulses.
Medicare and TennCare do not reimburse for such acupuncture devices, nor do Medicare and TennCare reimburse for P-Stim as a neurostimulator or as implantation of neurostimulator electrodes.
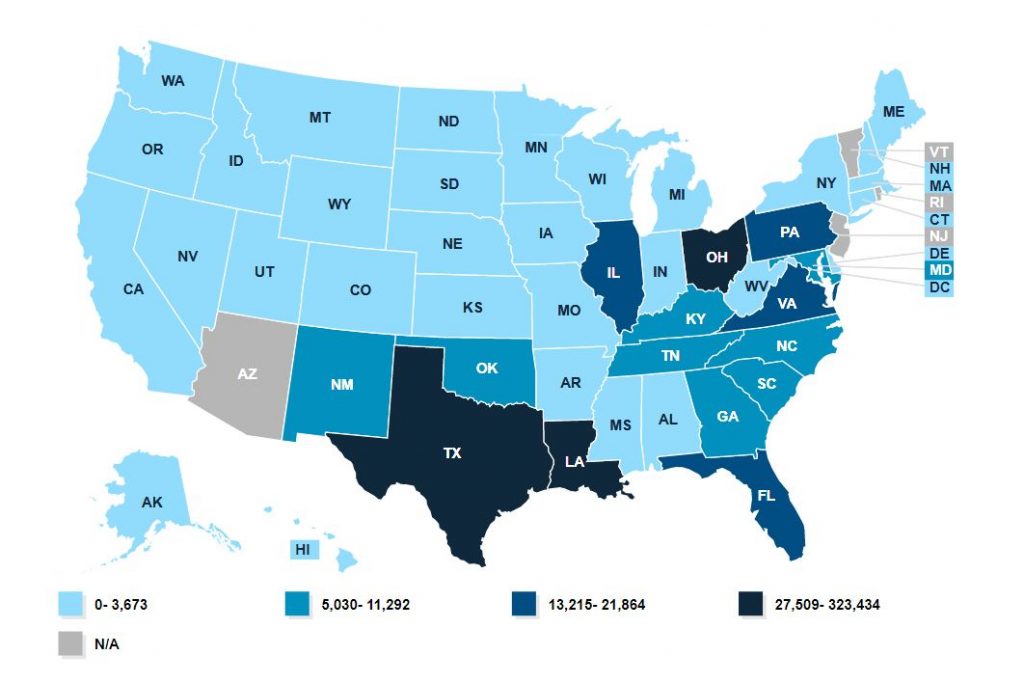
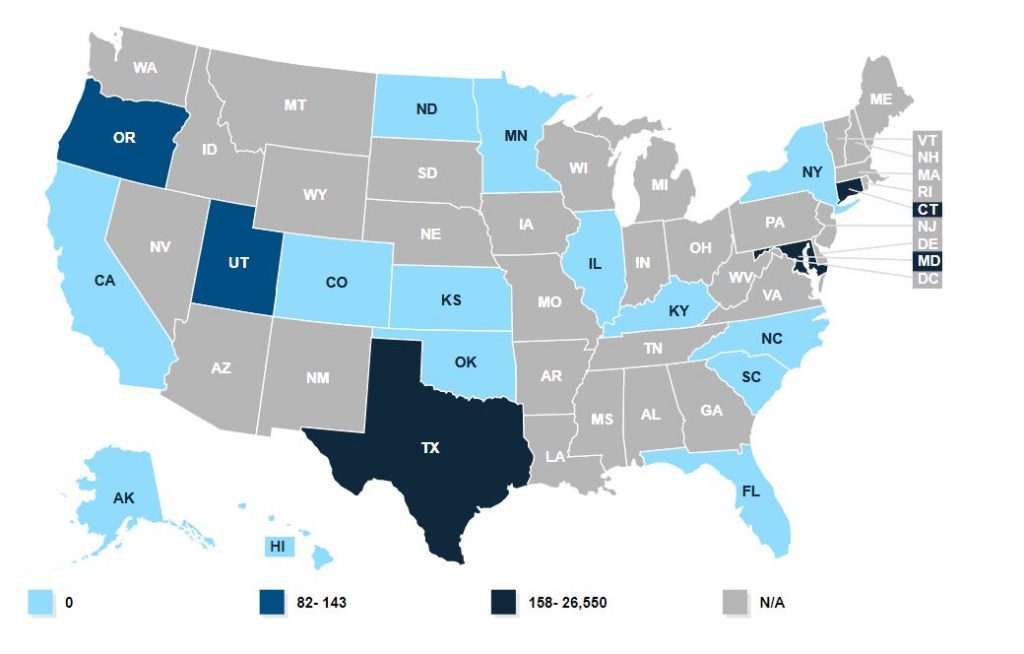
From May 2016 through November 2018, Dr. Anderson, Total Family, and Chiro2Med billed for, and were reimbursed by the United States for acupuncture using P-Stim devices under HCPCS Code L8679, which instead requires implantation of a neurostimulator with anesthesia in a surgical setting by a physician, typically a surgeon. Dr. Anderson, Total Family, and Chiro2Med separately billed for, and were reimbursed by, Medicare and/or TennCare for these devices over a two year period.
On June 10, 2020, Tennessee brought suit in the Chancery Court of Davidson County against Dr. Anderson under the Tennessee Medicaid False Claims Act for the false claims he submitted to TennCare.
Under the terms of the settlement, Dr. Anderson agreed to pay $1 million to the United States and Tennessee over five years.
Dr. Anderson also agreed to enter into an Integrity Agreement with the Office of Inspector General of the U.S. Department of Health and Human Services that will require regular monitoring of its billing practices for a period of three years.
Dr. Spencer and Total Family agreed to pay the United States $700,000 over five years.
Dr. Shea and Chiro2Med agreed to pay the United States $20,000 over five years.
“These settlements are part of a nationwide effort to hold accountable those providers who were paid improperly for non-reimbursable acupuncture under the guise of a surgically implanted neurostimulator,” said U.S. Attorney Cochran. “Working closely with our partners at CMS’s Center for Program Integrity, the Department of Health and Human Services Office of the Inspector General, our sister U.S. Attorney’s Offices, and the Tennessee Attorney General’s Office, we were able to identify those who profited from the submission of these false claims and negotiate resolutions that resulted in a significant recovery of taxpayer dollars.”
“This Office will not tolerate medical device fraud in Tennessee, whether it is the P-Stim as in these cases, or any type of fraud,” said General Slatery.
These cases were handled by the United States Attorney’s Office for the Middle District of Tennessee and the Tennessee Attorney General’s Office, Medicaid Fraud and Integrity Division, with assistance from the Tennessee Bureau of Investigation Medicaid Fraud Control Unit and the Department of Health and Human Services, Office of Inspector General. Assistant U.S. Attorney Kara F. Sweet represented the United States. Deputy Attorney General Tony Hullender represented Tennessee.
Clipped from: https://www.wsmv.com/news/the-u-s-and-tennessee-resolve-claims-worth-1-72-million/article_5155c642-4ed3-11eb-8c84-03fb1e524dbc.html?block_id=998344