Category: Amazing Free Content
Medicaid Concepts: Transportation as a Social Determinant of Health

This is part of our Medicaid Concepts series, in which we provide a high level overview of key concepts in the Medicaid industry today.
What do we mean by transportation as a social determinant of health?
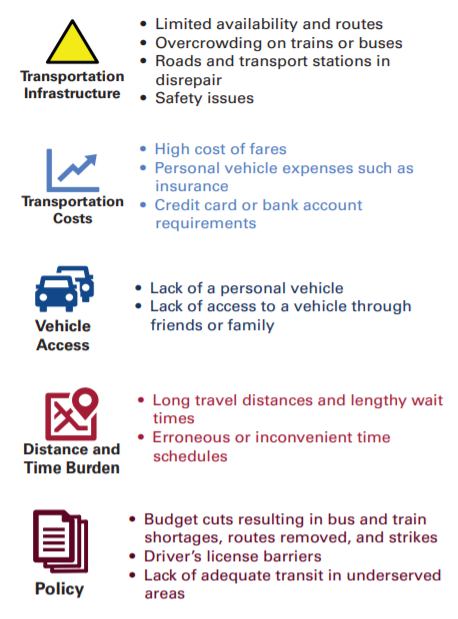
While most of the social determinants of health conversation focuses on various forms of food, clothing and shelter issues, lack of transportation is another area that is generally recognized as impacting healthcare. In places where public transportation is not available, the ability to get to health appointments can be especially limited. If a Medicaid member cannot actually get to the doctor’s appointment, then few of the benefits of proper care can be realized. According to a report from the American Hospital Association, more than 3.6M Americans do not get the care they need because they did have a way to get to their visit.
What role does Medicaid play?
Many Medicaid programs have operated optional non-emergency transportation (NET) programs for years. While these programs address the issue, there are long standing challenges with missed pickup appointments, overly complicated dispatch systems and legacy providers.
Several innovative Medicaid programs have emerged using rideshare vendors (like Uber and Lyft) to streamline the member experience and improve visit completion rates. Medicaid programs can partner with these vendors (or have their Medicaid managed care plans partner with them).
While these options can help meet gaps in urban environments, transportation challenges in rural areas for Medicaid members will likely require alternative solutions.
Explore further
http://www.hpoe.org/resources/ahahret-guides/3078
http://www.hpoe.org/Reports-HPOE/2017/sdoh-transportation-role-of-hospitals.pdf
https://www.ruralhealthinfo.org/topics/transportation
https://populationhealth.humana.com/social-determinants-of-health/lack-of-transportation/
5BF: 3/26/2021
Medicaid Concepts: Managed Long Term Services and Supports (MLTSS)
This is part of our Medicaid Concepts series, in which we provide a high level overview of key concepts in the Medicaid industry today.
What do we mean by Managed Long Term Services and Supports (MLTSS)?
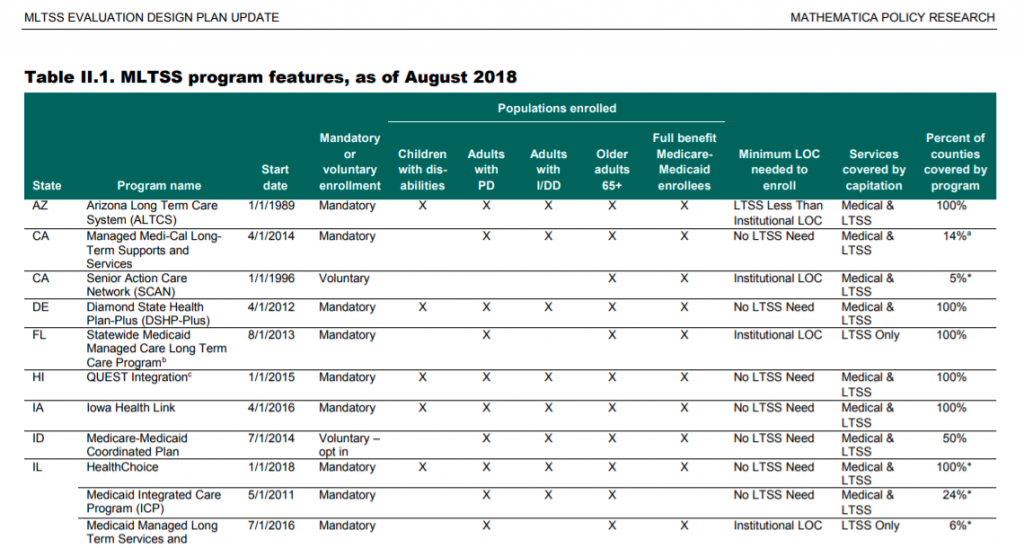
These are the services provided to Medicaid members in a managed care model. Because of the unique member needs, the focus on care coordination and management, and intense cost structure of this model many states have decided to use stand-alone managed care programs just for LTSS. The LTSS stands for long term services and supports. Add an “M” in front of it for “managed.”
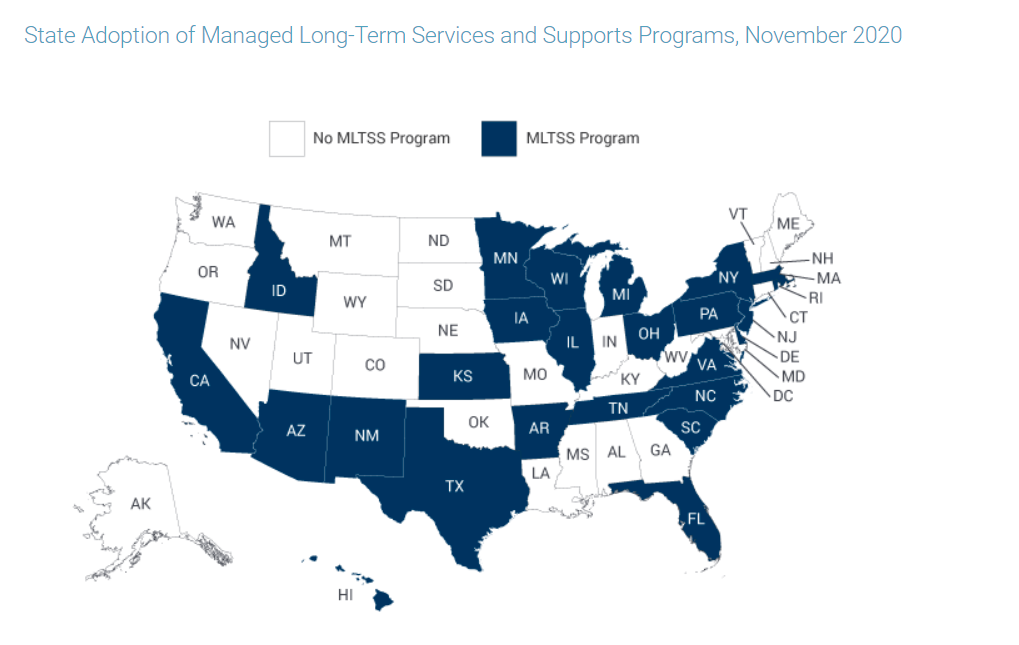
CMS has encouraged states to use MLTSS models with an array of funding efforts and aspirational goals. These include the Money Follows the Person (MFP) inititiative and the Balancing Incentive Program (where states are encouraged to increase the percentage of LTSS provided in the home or community vs. in a facility). These efforts have paid off- 25 states operate an MLTSS program as of November 2020 (compared to only 8 states in 2004).
Medicaid programs spent $167B on LTSS in 2016.
What role does Medicaid play?
States design the features of their MLTSS programs and contract with managed care companies to deliver the services. They also set eligibility requirements for members, which can include both functional and financial criteria.
States also work with plans and actuaries to set rates for these services.
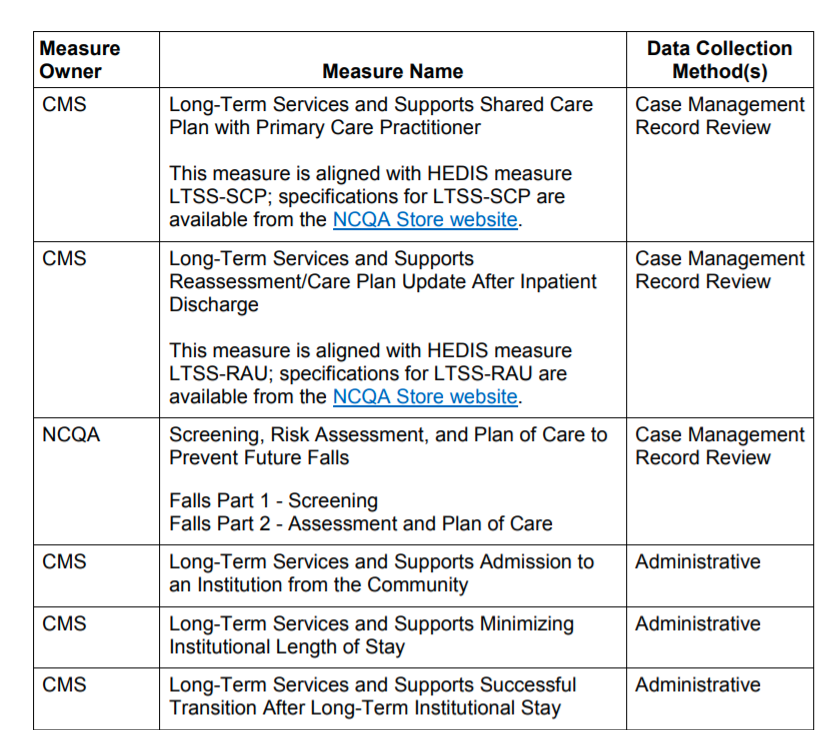
States also have to manage the quality reporting process for these services, using measures selected by CMS. These measures generally focus on ensuring needs assessments and care plan requirements are met.
Explore further
https://www.medicaid.gov/medicaid/managed-care/managed-long-term-services-and-supports/index.html
https://www.macpac.gov/subtopic/managed-long-term-services-and-supports
https://www.medicaid.gov/medicaid/downloads/final-eval-dsgn-mltss.pdf
https://www.medicaid.gov/medicaid/downloads/eval-dsgn-mltss.pdf
https://www.michigan.gov/mdhhs/0,5885,7-339-71547_4860_78446_78448-474121–,00.html
https://www.medicaid.gov/medicaid/downloads/mltss_assess_care_plan_tech_specs.pdf
https://www.nj.gov/humanservices/dmahs/home/mltss.html
https://www.macpac.gov/subtopic/eligibility-for-long-term-services-and-supports/
http://mltss.org/wp-content/uploads/2019/12/MLTSS-Profile-12-9-19.pdf
https://www.medicaidinnovation.org/_images/content/2019-IMI-MLTSS_in_Medicaid-Report.pdf
Medicaid Conversations: NAMD Medicaid Forward initiative with Matt Salo

Medicaid Concepts: Value-Based Payment Models
This is part of our Medicaid Concepts series, in which we provide a high level overview of key concepts in the Medicaid industry today.
What do we mean by value-based payment?
Defining value-based care / payment remains one of the largest challenges in all of the healthcare space, and Medicaid is no different. While everyone agrees that the concept means something akin to “pay more for better outcomes,” providers and payers continue to struggle to arrive at agreement on definitions, how to adjust for population mix and what incentives actually work.
Some terms you may hear related to value-based payment include: shared savings, gain sharing, risk corridors, incentives, withholds and pay for performance.
A sub-industry of solution vendors leverages the focus on value-based payments to drive sales and growth. These range from care management companies and specialized provider groups that use HEDIS performance as core to their value proposition, all the way up to software companies that have emerged to help providers keep track of the complex set of requirements in their value based contracts.
On the Medicare side, CMS implemented several value based programs meant to change the way providers are paid (as part of ACA). The most recent ones were rolled out in 2019: Alternative Payment Models (APMs) and the Merit-based Incentive Payment System (MIPS).
What role does Medicaid play?
Medicaid programs have also invested significant effort in migrating from the legacy fee for service system to value-based payment models. Early efforts included health homes and patient-centered medical homes (PCMH).
More recent efforts have attempted to leverage managed care plans to hold providers accountable for quality. Most states use HEDIS-based incentive systems for managed care payments. Many states require health plans to place an increasing percentage of their provider payments in value-based contracts. In these arrangements, the Medicaid agency establishes benchmarks and contracts with an External Quality Review Organization (EQRO) to oversee the plan performance.
States also have implemented innovative solutions separate from their managed care arrangements. Tennessee has a mature episode-based payment program that rewards providers for better outcomes on comprehensive bundles.
A few states have attempted to use Medicaid Accountable Care Organizations (ACOs). Many states also participated in the CMS-funded State Innovation Models (SIM) program to pilot new ways to use value-based payment approaches.
Explore further
https://www.medicaid.gov/Federal-Policy-Guidance/Downloads/smd20004.pdf
https://www.ama-assn.org/system/files/2019-04/medicaid-value-based-care-models.pdf
5BF: 3/19/2021
Senate confirms Xavier Becerra as HHS secretary
MM Curator summary
Becerra has been confirmed to head HHS.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
Key Points
- The Senate confirmed Xavier Becerra as Health and Human Services secretary.
- The California attorney general and former U.S. representative will have a major role in the Covid-19 vaccine rollout as the country tries to achieve a level of normalcy by the summer.
- Becerra will also play a part in the Biden administration’s plans to create a Medicare-like public health-care option.
- The confirmation vote was close, as Republicans have questioned Becerra’s health experience and previous support for “Medicare for All.”
Xavier Becerra, nominee for Secretary of Health and Human Services, answers questions during his Senate Finance Committee nomination hearing on Capitol Hill in Washington, DC, February 24, 2021.
Greg Nash | Pool | Reuters
The Senate confirmed Xavier Becerra as Health and Human Services secretary on Thursday as the U.S. aims to contain Covid-19 and achieve a semblance of normal life by summer.
Becerra, California’s attorney general, won approval by a narrow 50-49 margin in a Senate evenly split by party. Nearly all Republicans opposed the former U.S. representative’s nomination, questioning his health-care experience and past support for “Medicare for All.”
Becerra will be the first Latino to lead HHS. In a tweeted statement following his confirmation, Becerra said he is “honored and humbled by today’s vote” and “ready to get to work.”
The support of Sen. Susan Collins, a Maine Republican, removed the need for Vice President Kamala Harris to cast a tiebreaking vote.
Becerra will take a major role in one of the federal government’s most daunting undertakings ever. HHS will help to facilitate Covid-19 vaccinations and testing efforts as health officials hope widespread inoculation will beat back a mutating virus and allow businesses and schools to reopen.
While the virus’s spread has slowed in the U.S., the country is recording about 54,800 Covid-19 cases and at least 1,200 deaths every day, according to a seven-day average calculated by CNBC. About 15.5% of adults, and 37.6% of people over 65, are fully vaccinated, according to the Centers for Disease Control and Prevention.
Becerra will also have a prominent part to play if and when the Biden administration moves on to health-care reform. President Joe Biden has backed the creation of a Medicare-like public insurance option and changes to control the cost of drugs and care.
Ahead of the vote, Senate Majority Leader Chuck Schumer, D-N.Y., said Becerra “has decades of standing up for working-and middle-class Americans in Congress, fighting to protect and expand Medicare, Medicaid, and working to safeguard our health care system from attacks by the Trump administration.”
Becerra became the 20th member of the president’s Cabinet confirmed by the Senate. The chamber has turned its attention to filling out the executive branch since its passage of the $1.9 trillion coronavirus relief bill earlier this month.
Speaking at a Senate confirmation hearing last month, Becerra said he understands “the enormous challenges before us.” He said he would work not only to contain the virus but also to boost access to affordable health care.
Becerra touted his work as California’s attorney general to make Covid treatments more widely available and crack down on opioid manufacturers.
He succeeded Harris as the largest U.S. state’s top law enforcement official in 2017 after her election to the Senate the previous year. Becerra won a four-year term in 2018.
He represented California in the U.S. House from 1993 to 2017.
Clipped from: https://www.cnbc.com/2021/03/18/senate-to-confirm-xavier-becerra-as-hhs-secretary.html

Gov. Cox names Interim Medicaid Director
MM Curator summary
Utah has a new interim Medicaid Director.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
Utah Department of Health | Mar 17, 2021
The Utah Department of Health (UDOH) today announced Gov. Spencer Cox has appointed Emma Chacon as the Interim State Medicaid Director.
Chacon will be replacing Nathan Checketts who has served as Medicaid director for the past five years. In addition to overseeing the Medicaid program, Checketts also served as the deputy director of the UDOH. Checketts will be joining the Utah Department of Human Services (DHS) as a deputy director.
Chacon brings years of public service experience, having served as Medicaid deputy director and operations director, as well as other positions within the agency since 2005. Prior to her service within Medicaid, Chacon was the director of the Office of Recovery Services for 12 years, in addition to nearly 25 years at DHS.
“As Medicaid director, Nate Checketts worked tirelessly to ensure Utah’s most vulnerable populations remained the focus of the Medicaid program, while still being a good steward of funds provided by the taxpayer,” said Rich Saunders, executive director of the UDOH. “We are fortunate to have Emma Chacon continue to lead such a complex program with her expertise and dedication. Medicaid will continue to be in good hands, especially under the current pandemic circumstances.”
Medicaid is one of the largest programs in state government and contributes significantly to the financing of Utah’s health care system. Medicaid has an operating budget of more than $4.5 billion, and through its many programs provides more than 410,000 Utahns access to health care every year.
This press release was provided by the Utah Department of Health.
Clipped from: https://stateofreform.com/featured/2021/03/gov-cox-names-interim-medicaid-director/

Florida unlikely to expand Medicaid for 800,000 residents, despite offer of more federal money
MM Curator summary
Florida is not being swayed by the new expansion funding being offered.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
TALLAHASSEE — Gov. Ron DeSantis and Florida legislative leaders still aren’t interested in expanding Medicaid under the Affordable Care Act, despite the federal government’s offer to defray the cost to the state for two years as part of the $1.9 trillion COVID-19 relief package signed by President Biden last week.
Democrats and advocates who’ve pushed for expansion say there’s no excuse not to offer coverage to 800,000 more Floridians now that the cost to the state would be less.
Sen. Annette Taddeo, D-Miami, for example, noted that DeSantis doesn’t plan on giving back to the federal government any of the $10 billion in direct aid Florida is getting, as U.S. Sen. Rick Scott requested, so traditional GOP arguments in favor of fiscal restraint seem to have evaporated in Tallahassee, she said.
“Even Gov. DeSantis said to former governor and senator Rick Scott, ‘that’s crazy to turn back money,'” Taddeo said Wednesday. “Well, I feel exactly the same way — that’s crazy to turn back money for Medicaid expansion in the middle of a global pandemic, to say to people, ‘you still can’t have insurance.'”
Medicaid expansion would provide coverage under the program, which is run jointly by the state and federal government and covers poor families, children and pregnant women, to people who earn up to 138% of the federal poverty line, which stands at $18,000 per year for a person and $37,000 for a family of four.
The federal government would cover the entire cost of expansion at first before their share reduces to 90%, with the state paying the remaining 10%. The usual cost share of the current Medicaid program varies by year but can reach as high as 60% paid by the federal government and 40% paid by Florida.
Under the relief package, for two years the federal government would pay an extra 5% of its share of the main Medicaid program, which is expected to serve nearly 4.6 million Floridians next fiscal year before enrollment drops in future years due to a rebounding economy.
Florida’s Medicaid program is projected to cost $31.6 billion this year, or about one-third of the state’s $92.2 billion budget. State economists estimate the state’s share this year to be $11 billion and it is expected to rise to $13 billion next year.
Florida Policy Institute, a liberal think tank based in Orlando, estimates expanding Medicaid now would save the state $3.5 billion.
That would free up money for other things, such as education and the environment, and advocates argue the savings would be even greater, because the cost of uncompensated care at hospitals would go down, eventually reducing health care premiums across the entire system.
“There is no excuse fiscally for any lawmaker to say it would be fiscally undoable,” said Holly Bullard, FPI chief strategy and development officer. “The fiscal argument isn’t there, it’s really reversed.”
But GOP leaders still have an eye on the 10% cost to the state in future years.
“The president has concerns about the long-term, recurring costs associated with Medicaid expansion,” Katie Betta, spokeswoman for Senate President Wilton Simpson, R-Trilby, stated in an email explaining his opposition.
DeSantis office didn’t return a request for comment Wednesday, but his spokeswoman told the Washington Post this week he “remains opposed to the expansion of Medicaid in Florida.”
House Speaker Chris Sprowls, R-Palm Harbor, is more concerned about allowing more residents coverage, an echo of the criticism from past GOP House leaders that “able-bodied adults” would be eligible for Medicaid under expansion.
“The Speaker will not pursue a Medicaid expansion,” Sprowls spokeswoman Jenna Sarkissian stated in an email. “He believes Medicaid should be reserved for our most vulnerable residents, such as low-income senior citizens, people with disabilities, children and pregnant women.”
Sarkissian added that Sprowls “has expressed a strong desire to address disparities in maternal health care for low-income women and invest in areas like career and higher education help to generate better outcomes for Floridians and put them on a path to employment, financial resilience and prosperity.”
After years of intense debate over Medicaid expansion, the fight over the issue in the Legislature has cooled.
In 2013, Florida House Democrats demanded all bills be read in full, slowing down the chamber to protest the lack of action on the issue, but a Senate plan to allow newly eligible enrollees to receive private health plans paid by the federal government was rebuffed by House Republicans.
At the time, then-Gov. Rick Scott had come out in favor of expansion, as long as the federal government was covering the costs. After he was reelected in 2014, he reversed course and didn’t speak in favor of a plan pushed by Senate Republicans in 2015 to expand Medicaid while imposing work requirements and attaching other strings. House Republicans again rejected the plan, but only after a standoff between the chambers that delayed the budget.
Faced with the stalemate in the Legislature, those in favor of expansion have turned to a potential ballot measure that would put the issue before voters. Those efforts, however, have been stymied so far, too.
The Florida Decides Healthcare political committee halted its petition gathering push in 2019, saying it would be unable to gather enough petitions in time to be placed on the 2020 ballot. The group will try again for the 2022 ballot, but the Legislature last year passed a law placing greater requirements on petition gatherers and increased the amount of petitions needed for a Florida Supreme Court review.
Taddeo wants the Legislature to eliminate the need for that process by putting the measure on the ballot itself. She’s filed SJR 276 to put Medicaid expansion on the 2020 ballot, but that avenue is unlikely, too, because it requires 60% support in both chambers.
“After this icing on the cake is handed to us from the federal government … and we still don’t do it – it’s so sad because we’re playing with people’s lives,” Taddeo said.
Clipped from: https://www.orlandosentinel.com/politics/os-ne-florida-medicaid-expansion-20210317-uxyqvh3trjgvthw4qxoba52syy-story.html