Helping you consider differing viewpoints. Before it’s illegal.
Article 1:
NTU Leads Coalition Letter to Combat Fraud in Federal Health Care Programs, Pete Seep, July 19, 2018
Clay’s summary: Makes a strong case for using “smart cards” for the Medicaid benefit… Worth a read.
Key Passage from the Article
Federal health care programs have long been plagued by improper payments, one component of which is attributable to fraudulent activities such as identity theft, billing for services never rendered, or falsifying patient records to obtain prescription drugs illicitly. A 2012 study led by former Director of the Centers for Medicare and Medicaid Services Donald Berwick pegged the fraud rate alone (as opposed to other types of improper payments) in Medicare and Medicaid at between 3 percent and 10 percent of all dollars spent. Taxpayers may be forgiven for thinking that the higher figure might be the more plausible one.
Furthermore, although the extent of such fraud is not precisely known, existing research suggests that policymakers seem likelier to understate rather than overstate its prevalence. For example, the Government Accountability Office (GAO) recently concluded that existing improper payment identification methods failed to find some $200 million in misspent funds within Medicaid’s Managed Care Organizations.
A variety of responses are required to reduce improper payments in federal programs, but one of the more promising — and least controversial — remedies should be smart card technology. HR 4554 aims to create a pilot program within Medicare employing “secure, electronic authentication of the identity of a Medicare beneficiary at the point of service through a combination of the smart card and a personal identification number known by or associated with such beneficiary.” The result would be a system highly resistant to ID theft, with sufficient data capacity on each beneficiary’s card to significantly reduce other undesirable outcomes such as prescription abuse. The latter concern is especially timely, given the need to deploy as many policy assets as possible in reducing the severity of opioid addiction (and therefore additional taxpayer burdens associated with treatment and emergency responses).
…
Article 2:
California Medicaid shows Obamacare failure, Oklahoman Editorial Board, August 23, 2018
Clay’s summary: That’s a mean headline. Must not be true. Phew! Almost had to challenge my own strongly held beliefs there for a minute!
Key Passage from the Article
Among other things, passage of the Affordable Care Act was supposed to dramatically reduce non-emergency use of ERs. Because more people would have coverage, fewer would delay routine care and they would be less likely to use an ER to get cold medicine or similar treatments. A recent study in California illustrates there was a huge gap between that theory and reality. California’s Democrat-dominated state government eagerly embraced the ACA by expanding the Medicaid program, which is the main method the law used to reduce the uninsured rate. A new report by the California Health Care Almanac, an online clearinghouse for data and analysis, shows Medicaid expansion resulted in no obvious reduction in unnecessary ER visits. In fact, a slight acceleration in the use of ERs occurred. In 2006, there were 10.1 ER visits per 1,000 people in California. By 2016, that rate had increased to 14.6. Contrary to activists’ predictions, the steady increase in ER use observed before Medicaid expansion did not turn into a decline after expansion. The report notes the number of ER visits by Medicaid patients “almost doubled between 2006 and 2016,” rising from 23 percent of patients in 2006 to 43 percent by 2016. That increase is far larger than the reduction in self-pay/uninsured visits, which declined from 16 percent of patients to 7 percent.
Article 3:
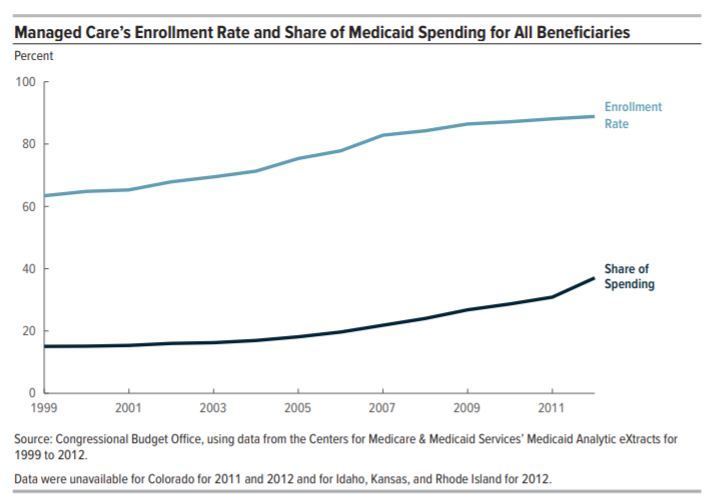
Exploring the Growth of Medicaid Managed Care
Clay’s summary: Had no idea CBO did these reports. Great charts that I will be using in my next conference talks for sure.
Key Passage from the Article
In this case its a chart. Note the enrollment line slowing in recent years, but the spending line turning up..
Lots of good discussion possible as to why: increase in federal spending incentives more spending per bennie (ACA), sicker / more vulnerable bennies being put into managed care, plans getting better at cap negotiation, etc..