MM Curator summary
The revised AR expansion waiver has back-pedaled its original design to include no requirements related to work, but still has different benefits for members who do not engage in their own health.
The article below has been highlighted and summarized by our research team. It is provided here for member convenience as part of our Curator service.
HUTCHINSON (file photo) Asa Hutchinson
Governor Hutchinson said Tuesday at his press conference that he anticipates that the federal government will approve the state’s request to renew its Medicaid expansion program, with some revisions, prior to the end of the year, when the state’s current Medicaid expansion agreement expires.
The Medicaid expansion, authorized by the federal Affordable Care Act, covers adults who make less than 138 percent of the federal poverty level (an annual income of $17,774 for an individual or $36,570 for a family of four). The program in Arkansas, first enacted in 2014, uniquely uses Medicaid funds to pay for private health insurance to cover most beneficiaries. Once nicknamed the “private option” and now known as “Arkansas Works,” it was implemented under a series of agreements with the federal government, known as waivers because the feds waive certain Medicaid rules. The latest request, submitted this summer, renames the program ARHOME.
“We’ve been assured that they would act on that in sufficient time so the waiver doesn’t expire — which is the end of the year,” Hutchinson said. “So our [Department of Human Services] is working diligently with them on that. I don’t anticipate any issue in getting the new waiver granted. But that specific timeframe is undetermined.”
The new waiver request maintains the use of private health insurance to cover beneficiaries, but would route people who are “inactive” to the regular Medicaid program rather than the private plan. Under the state’s waiver request, it doesn’t take much to stay “active” — if beneficiaries simply choose their own plan as opposed to being auto-assigned, or if they go to the doctor for a checkup, they are considered active, even if they don’t participate in other incentive programs the state is planning (participating in one of those programs, which includes incentives to encourage employment, would also count). So long as they interact with the plan in some way — completing a health assessment, say, or any use of a medical service, etc. — they can stay in the private plan. In very early talks with lawmakers, the idea was floated of making incentives around work or education/training part of the requirement to keep a private plan. But the final framework only designates someone as inactive if they don’t do anything at all related to their health care plan.
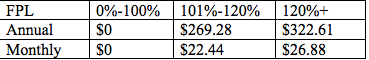
The ARHOME waiver also proposes an increase in premiums charged to most beneficiaries who make more than the poverty level. Beneficiaries would not lose coverage for failure to pay, but would incur a debt to the insurance companies (currently, those who fail to pay premiums incur a debt to the state, which can be withheld from tax refunds). Currently, most beneficiaries who make more than the poverty line are charged a flat $13 per month. The ARHOME waiver proposes bumping that up, depending on income:
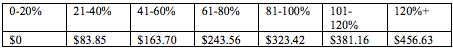
Co-payments would also be higher, and would be applied to more beneficiaries. Currently, co-payments are only charged to beneficiaries who make more than the poverty line, and are capped at $60 per quarter. Under ARHOME, they would be charged at most income levels and the caps would be bumped up (see chart below). Failure to pay would incur a debt to the provider. No one would lose coverage for failure to pay. According to the waiver request, “A provider cannot refuse to provide service for non-payment at the first occurrence but can refuse to provide a future service due to non-payment.” Here are the proposed maximum annual allowable amounts on the co-pays by income:
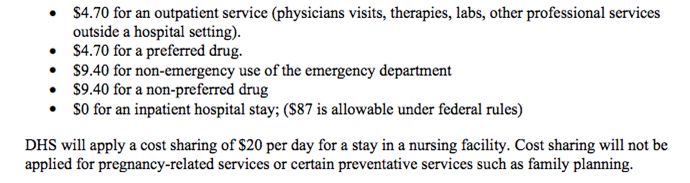
Here are the co-pays that will be in place in 2022, according to the waiver proposal:
Advertisement
The total of both co-pays and premiums will be capped at 5 percent of household income per quarter.
Those deemed medically frail — and those routed in a new program for people with serious mental illness or substance use disorder — will not be charged premiums or co-pays.
The ARHOME program also includes new initiatives for rural health, maternal and infant health, behavioral health and certain at-risk populations. State officials focused on these initiatives when they unveiled the waiver request last summer.
ARHOME also includes wellness incentives programs, along with the work and education incentives programs, as well as mechanisms to contain cost growth and to establish quality performance targets for the private plans.
If the feds approve the ARHOME waiver, it could still come with minor variations to the framework not described in the request: Certain terms and conditions may apply that will provide more details about just how that framework will function in practice.
